Premium Only Content
Impact of Childhood Vaccination on Short and Long-Term Chronic Health, a Puke(TM) Audiopaper
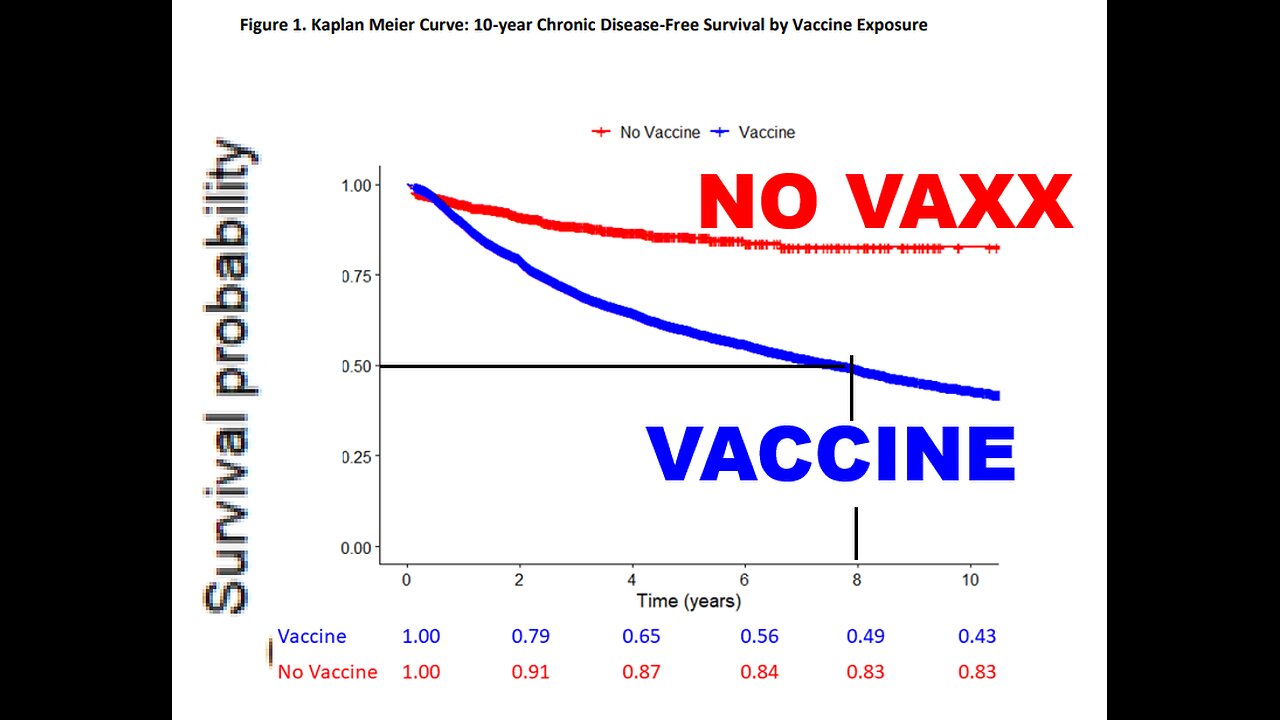
In other words, according to figure one of this study, your child has a 50-50 chance of developing a chronic disorder within 8 years.
This may be potentially cumulative, meaning a 75 percent chance within 16 years of vaccination.
Index of Other Science Articles:
https://rumble.com/v3t4yzj-index-of-science.-music-by-dan-vasc.html
Impact of Childhood Vaccination on Short and Long-Term Chronic Health Outcomes in Children: A Birth Cohort Study.
Lois Lamerato, and others.
Henry Ford Health System, Detroit Michigan.
Running head: Association of childhood vaccination on chronic health in children.
Abstract.
Objective: To compare the short and long-term health outcomes, within a captured payer environment, of children exposed to one or more vaccines to those unexposed.
Design: Birth cohort study.
Setting: Integrated healthcare system in Michigan.
Participants: 18,468 children born between the years two thousand and twenty-sixteen enrolled in the health system insurance plan.
Main Outcome Measures: Development of a chronic health condition over time.
Results:
A total of 18,468 consecutive subjects met eligibility criteria for the study, of which 1,957 had no exposure to vaccination and 16,511 had received at least one vaccine during their enrollment in the plan with various levels of exposure.
After multivariate adjustment, Cox proportional hazards modeling demonstrated that exposure to vaccination was independently associated with an increased risk of developing a chronic health condition (Hazard Ratio 2.53, Confidence Interval 2.16 to 2.96).
Of the chronic health conditions, exposure to vaccination was independently associated with an increased risk of asthma (Hazard Ratio 4.25, Confidence Interval 3.23 to 5.59),
Autoimmune disease (Hazard Ratio 4.79, Confidence Interval 1.36 to 16.94),
Atopic disease (Hazard Ratio 3.03, Confidence Interval 2.01 to 4.57,
Eczema (Hazard Ratio 1.31, Confidence Interval 1.13 to 1.52, and
Neurodevelopmental disorder (Hazard Ratio 5.53, Confidence Interval 2.91 to 10.51).
There were no chronic health conditions associated with an increased risk in the unexposed group. The overall probability of being free of a chronic health condition at 10-years of follow up was 43 percent in the group exposed to vaccination and 83 percent in the unexposed group.
Conclusion:
This study found that exposure to vaccination was independently associated with an overall 2.5-fold increase in the likelihood of developing a chronic health condition, when compared to children unexposed to vaccination. This association was primarily driven by asthma, atopic disease, eczema, autoimmune disease and neurodevelopmental disorders. This suggests that in certain children, exposure to vaccination may increase the likelihood of developing a chronic health condition, particularly for one of these conditions.
Introduction.
Over the past 30 years, the prevalence of chronic health conditions in children has increased.
According to a twenty-eleven study, approximately 43 percent of children in the United States, 32 million, have at least 1 of the 20 chronic health conditions assessed in the study. Despite this, there is a paucity of published data to determine contributing factors.
Vaccination has reduced the incidence of certain targeted childhood infections and their associated morbidity and mortality. Nonetheless, vaccine hesitancy remains a significant barrier to maintaining and increasing vaccine uptake and the number of parents foregoing all vaccinations has been increasing. Common parental concerns relate to the growth of the vaccine schedule, administering multiple vaccines contemporaneously, and the potential for long-term adverse health outcomes from vaccination. Research addressing these vaccine safety concerns can assist clinicians in discussions with their patients and serve to reassure parents of the overall safety of vaccination.
The safety review period in pre-licensure clinical trials is typically of insufficient duration, less than 30 days, to assess a vaccine’s impact on long-term health outcomes. However, a number of post-licensure observational studies have, with mixed results, examined whether certain vaccines are associated with developing certain health conditions. An important limitation to these studies, as highlighted by the Institute of Medicine (IOM) report, The Childhood Immunization Schedule and Safety, is that “most vaccine-related research focuses on the outcomes of single immunizations or combinations of vaccines administered at a single visit,” instead of comparing completely unvaccinated populations with those receiving one or more vaccines. This led the IOM to recommend retrospective studies evaluating the health outcomes of vaccinated versus unvaccinated populations.
Hence, this study compared the short and long-term health outcomes, within a captured payer environment, of children unexposed to vaccines with those exposed to one or more vaccines. Addressing this significant data gap could allay parental concerns and bolster vaccine confidence.
Methods.
Study Setting.
Henry Ford Health System (HFHS) is a large, vertically integrated healthcare system, offering primary, pediatric, acute, and specialty services in Metropolitan Detroit, with 4.2 million ambulatory care visits annually. The Health Alliance Plan (HAP), a non-profit health maintenance organization (HMO) and subsidiary of HFHS, has approximately 570,000 enrolled members, approximately one-third of whom receive care within HFHS. HFHS’s diverse patient population, clinical resources and information technology systems, make it uniquely suited for this study.
Study Design.
This retrospective study evaluated health outcomes of a consecutive cohort of children born between two thousand and twenty-sixteen and enrolled in HAP. This cohort was identified using the HAP and HFHS administrative database. Subjects were observed from birth until the earlier of disenrollment in the plan or December 31, twenty-seventeen. Data sources for this study included medical, clinical and payer records from HFHS and HAP, supplemented with data from the State of Michigan immunization registry. Data tables included encounters (outpatient and emergency), hospitalizations, diagnoses, procedures and billing data on all services. Vaccinations evaluated included all vaccines on the Centers for Disease Control and Prevention (CDC) Recommended Child and Adolescent Immunization Schedule (Vaccine Schedule). Death data was obtained from HFHS electronic medical records and the State of Michigan’s Vital Records System and manual chart review was conducted to ascertain cause of death for subjects who died during plan enrollment. All HFHS patients receive a lifetime medical record number that links across data-tables.
The study was reviewed and approved by HFHS’s Institutional Review Board and conducted in accordance with the International Society for Pharmaco-epidemiology’s Guidelines for Good Pharmaco-epidemiology Practices.
Study Population.
Inclusion criteria: born and enrolled in HAP for greater than 60 days between January 1, two thousand and December 31, twenty-sixteen with HFHS designated as their primary care system.
Exclusion criteria: chromosomal abnormalities, cerebral palsy, cystic fibrosis, spina bifida, congenital heart disease, or brain, neurological, or other congenital conditions present or discovered after birth.
These exclusions correspond with the objective of evaluating long-term health outcomes in a generally healthy birth cohort.
Definitions and Outcomes Assessment.
The primary outcome of this study was a chronic health composite outcome which included conditions identified by the Child and Adolescent Health Measurement Initiative, and augmented with conditions considered to be of public concern or public health significance in the CDC’s White Paper on Studying the Safety of the Childhood Immunization Schedule. The composite includes: diabetes, asthma, food allergy, cancer, brain dysfunction, atopic and autoimmune disease, and neurological, neurodevelopmental, seizure and mental health disorder. A subject with one or more of these was classified as having a chronic health condition. Other health conditions evaluated, but not part of the composite, include asthma attack or bronchospasm, anaphylaxis, eczema (acute and chronic), ear infection (acute and chronic) and peanut allergy.
We identified the relevant International Classification of Diseases, Ninth and Tenth Revision (ICD-9-CM and ICD-10-CM) diagnoses from healthcare encounters during enrollment in the plan for the conditions of interest. Subjects were classified by exposure to immunizations prior to onset of each condition, exposed versus unexposed, and then compared based on exposure status.
Brain dysfunction was defined as encephalopathy or encephalitis. Neurodevelopmental disorders were defined as autism, tics, ADD ADHD, developmental delay, speech disorder, and learning, motor, intellectual, behavioral, and other psychological disability. Mental health disorder was defined as anxiety, depression, bipolar, phobia, emotional disturbance, psychosis, somatoform, and eating, manic, mental, mood, obsessive compulsive, personality, and stress adjustment disorder. Only children 2 years and older were evaluated for neurodevelopmental and mental health disorders. Chronic eczema was defined as at least 1 reoccurrence 60 days or more after first episode. Chronic ear infection was defined as at least 2 reoccurrences within a year after first episode.
Statistical Analysis.
Descriptive characteristics are reported as percentages, mean values plus or minus standard deviations, or median values with interquartile ranges, IQR’s.
Chi-square tests were used to compare the difference in baseline characteristics differences between vaccinated and unvaccinated children at birth. The number of events for each outcome and incidence rate per million patient-years were calculated.
Incidence-rate-ratios, calculated by Poisson regression models, are presented with their associated 95 percent confidence intervals. Univariate and multivariate Cox proportional-hazards models were used to evaluate the association between health outcomes and vaccination status. The Kaplan-Meier method was used to estimate the 10-year cumulative risk of developing a chronic health condition from birth to the first episode of the condition and classified by prior exposure to immunization (exposed versus unexposed). The groups were compared with the use of a log-rank test. A P-value of less than 0.05 was considered statistically significant.
Since enrollment time was shorter overall in the unexposed group, sensitivity analyses were conducted by repeating the above analyses for subjects enrolled for at least 1-year, 3-years and 5-years. Additionally, to overcome potential ascertainment bias in subjects with lower levels of health care utilization, we conducted a sensitivity analysis by repeating the above analyses in only those subjects with at least one encounter at HFHS during plan enrollment.
Results.
Study Population.
A total of 18,468 consecutive subjects met eligibility criteria, of which 1,957 were unexposed and 16,511 were exposed to at least one vaccine, see Table 1. In exposed subjects, the median number of vaccinations was 18 (IQR 2 to 28). Characteristics more common in the exposed group were female sex, African American race, low-birthweight, prematurity, respiratory distress and trauma at birth. The median follow-up time was 904 (IQR 392 to 1,954) days for all subjects, 970 (IQR 430 to 2,093) days for exposed subjects, and 461 (IQR 196 to 1,081) days for unexposed subjects, with enrollment up to 6,575 days in the exposed group and 6,386 days in the unexposed group.
Clinical Outcomes.
Incidence rates and incidence rate ratios (IRR), based on exposure status prior to developing the condition, were calculated, see Table 2.
Overall, the development of a chronic health condition occurred more often in the group exposed versus unexposed to vaccination (277 versus 112 per million patient years, p less than 0.0001, and was more common in those exposed to vaccination (INCIDENCE RATE RATIO 2.48, Confidence Interval 2.12 to 2.91.
A statistically significant association was found between vaccination and the incidence of asthma, atopic and autoimmune disease, and mental health and neurodevelopmental disorders including developmental delay and speech disorder. A statistically significant association was not found between vaccine exposure and the incidence of cancer, food allergy, autism, motor disability, or neurological or seizure disorder.
Other conditions occurring more frequently in exposed subjects included:
Ear infection (INCIDENCE RATE RATIO 6.63, Confidence Interval 5.73 to 7.66),
Chronic ear infection (INCIDENCE RATE RATIO 5.67, Confidence Interval 4.37 to 7.37),
Anaphylaxis (INCIDENCE RATE RATIO 8.88, Confidence Interval 1.24 to 63.47),
And asthma attack or bronchospasm (INCIDENCE RATE RATIO 6.30, Confidence Interval 3.85 to 10.31).
Vaccine exposure was not associated with increased incidence of eczema (INCIDENCE RATE RATIO 1.06, Confidence Interval 0.91 to 1.23), chronic eczema (INCIDENCE RATE RATIO 0.94, Confidence Interval 0.74 to 1.20) or peanut allergy (INCIDENCE RATE RATIO 6.80, Confidence Interval 0.95 to 48.69).
After multivariate adjustment, Cox proportional hazards modeling demonstrated that exposure to vaccination was independently associated with an increased risk of developing a chronic health condition (Hazard Ratio 2.54, Confidence Interval 2.16 to 2.97), see Table 3. Vaccine exposure was independently associated with an increased risk of asthma, eczema, atopic and autoimmune disease, and neurodevelopmental disorders including developmental delay and speech disorder. Other variables in the model independently associated with increased risk of developing a chronic health disorder were: male gender (Hazard Ratio 1.33, Confidence Interval 1.26 to 1.41),
African American race (Hazard Ratio 1.11, Confidence Interval 1.04 to 1.18),
Low-birth-weight (Hazard Ratio 1.20, Confidence Interval 1.01 to 1.42),
Very-low-birth-weight (Hazard Ratio 1.48, Confidence Interval 1.14 to 1.91) and
Prematurity (Hazard Ratio 1.24, Confidence Interval 1.09 to 1.41).
Vaccine exposure was not significantly associated with higher risk for cancer, food allergy, autism, motor disability, or neurological, seizure or mental health disorder. Incident rate ratios and hazard ratios could not be calculated for brain dysfunction, diabetes, ADHD, tics, or behavioral, learning, intellectual, or other psychological disability since all cases occurred in the group exposed to vaccination and no cases occurred in the unexposed group.
Vaccine exposure was also independently associated with increased risk for developing other conditions, including:
Ear infection (Hazard Ratio 7.00, Confidence Interval 6.05 to 8.10),
Chronic ear infection (Hazard Ratio 7.89, Confidence Interval 6.08 to 10.24),
Anaphylaxis (Hazard Ratio 5.64, Confidence Interval 1.11 to 28.74),
Asthma attack or bronchospasm (Hazard Ratio 5.82, Confidence Interval 3.58 to 9.47) and
Eczema (Hazard Ratio 1.31, Confidence Interval 1.13 to 1.52).
Vaccine exposure was not associated with chronic eczema (Hazard Ratio 1.26, Confidence Interval 0.98 to 1.60) or peanut allergy (Hazard Ratio 6.31, Confidence Interval 0.88 to 45.37).
Time to event analysis demonstrated that the overall probability of being free of a chronic health condition at 10-years of follow up was 43 percent in the group exposed to vaccination and 83 percent in the unexposed group, log-rank test, p less than 0.0001, see Figure 1.
There were six deaths in the cohort during enrollment. After manual review of medical records, including death certificate where available, cause of death was determined to be due to a complicated clinical course from birth (2 exposed, 1 unexposed), brain injury (1 exposed), and unknown cause (2 exposed).
Sensitivity Analyses.
Since median enrollment time was shorter in the unexposed group, a sensitivity analysis for developing a chronic health condition was conducted for subjects enrolled in the health plan for at least 1-year, 3-years and 5-years which demonstrated consistent results. Vaccine exposure was associated with higher incidence of a chronic health condition for subjects enrolled at least:
1-year (INCIDENCE RATE RATIO 2.75, Confidence Interval 2.31 to 3.28),
3-years (INCIDENCE RATE RATIO 3.38, Confidence Interval 2.67 to 4.30), and
5-years (INCIDENCE RATE RATIO 4.09, Confidence Interval 2.84 to 5.90), as well as a higher risk for developing a chronic health condition for subjects enrolled at least:
1-year (Hazard Ratio 2.84, Confidence Interval 2.38 to 3.38),
3-years (Hazard Ratio 3.48, Confidence Interval 2.74 to 4.42), and
5-years (Hazard Ratio 4.05, Confidence Interval 2.82 to 5.83).
To address the potential for ascertainment bias in subjects with lower levels of health care utilization, we conducted a sensitivity analysis by repeating the above analyses using only subjects with at least one encounter during enrollment. Vaccine exposure was associated with higher incidence of a chronic health condition for subjects with at least one healthcare encounter (INCIDENCE RATE RATIO 1.83, Confidence Interval 1.56 to 2.14) as well as a higher risk for developing a chronic health condition (Hazard Ratio 1.87, Confidence Interval 1.60 to 2.19).
Discussion.
Main Findings.
This study is a comprehensive analysis to determine if exposure to vaccination is associated with the development of any long-term chronic health condition in children, or if outcomes are similar, or superior, to those unexposed. We did not find any statistical association between vaccine exposure and cancer, food allergy, autism, seizure disorder and certain other conditions. Statistical comparisons could not be conducted for certain conditions, such as diabetes and ADHD, because there were no cases in the unexposed group. Despite this and in contrast to our expectations, we found that exposure to vaccination was independently associated with an overall 2.5-fold increase in the likelihood of developing a chronic health condition, when compared to children unexposed to vaccination. This association was primarily driven by increased risk for asthma, atopy, eczema, autoimmune disease and neurodevelopmental disorders. Overall, our findings suggest that in certain children exposure to vaccination may increase the likelihood of developing a chronic health condition, particularly for one of these disorders.
Interpretation and comparison with previous studies.
Vaccines have contributed to reducing many targeted infections and their related morbidity and mortality, and are regarded as an important public health achievement of the last century.
The CDC’s Vaccine Schedule has evolved from five vaccines in nineteen ninety-four to 15 in twenty-twenty. Despite these advancements, there is a paucity of data evaluating the impact of vaccination on long-term health outcomes, whether beneficial or detrimental, particularly for immune-related conditions.
Limited by ethical guidelines, pre-and-post-licensure clinical trials for vaccines rarely include a comparator arm unexposed to vaccination. These trials also generally have a shorter safety review period, less than 30 days, which limits their ability to assess long-term outcomes. Observational studies can address these data gaps but, to date, have produced conflicting results. Some studies have found an association between vaccination and an increased risk of asthma, atopy, eczema, autoimmune disease and neurodevelopmental disorders, as found in this study.
Other studies have found no association.
A common and important limitation in this body of work is that almost all studies lack a truly unexposed comparator group, such as the one in this study, and hence typically evaluate receiving (vaccinated) versus not receiving one vaccine (unvaccinated) in a cohort that receives most other vaccinations (vaccinated).
For example, one study designed to evaluate the relationship between vaccination status (one or more versus none) and long-term health outcomes in children was a population-based parental survey conducted in Germany. Although limited by selection bias and parental recall, it found no statistical association of vaccination with atopy, eczema, or asthma.
However, the measure of vaccination was limited to certain vaccines, and the very small unexposed group may have been exposed to other vaccinations such as varicella, rotavirus, pneumococcal, meningococcal, influenza and or others.
According to the IOM twenty-thirteen, few studies have evaluated the Vaccine Schedule, or variations thereof, and its association with health outcomes and none have compared differences between entirely unvaccinated populations and those fully or partially vaccinated.
Our study, to our knowledge, is the first to compare multiple clinical outcomes over time between vaccinated (any vaccine) and completely unexposed children in a captured payer environment relying on diagnoses and vaccine status from medical records.
Biologic mechanisms elucidating how vaccine exposure in certain individuals might increase a health risk are unclear and beyond the scope of this study, but likely differ by condition, vaccine and recipient characteristics. A common theme in the literature is that vaccination may trigger a genetic and or immunologic susceptibility.
Vaccines aim to stimulate an antigen-specific immune response, however there are significant gaps in understanding the complex immunological mechanisms involved, and concern has been raised about potential untoward or off-target immunological effects in susceptible recipients.
According to an IOM report, epidemiologic and mechanistic research suggest that most individuals who experience an adverse response to a vaccine have a preexisting susceptibility due to genetic variants (in human or microbiome DNA), environmental exposures, behaviors, intervening illness, developmental stage or others. Viewed as an environmental exposure, in addition to antigens, vaccines also contain small amounts of preservatives, adjuvants, additives and residual substances from the manufacturing process. While this study cannot delineate the impact of epigenetics or a particular vaccine component, the unexposed group was not exposed to vaccine components, and the exposed group to one or more.
Epigenetics is an emerging field of study which explores how the environment can influence how genes are expressed without involving alterations in the DNA gene sequence. Research has shown that epigenetics may play a role in the pathogenesis of many diseases, including asthma, atopy, eczema, autoimmune disease and neurodevelopmental disorders, though precise etiologies vary and remain largely unknown. Genetically-mediated individual variations in the immunogenicity and reactivity of vaccines has been demonstrated.
The field of vaccine adversomics, though in its infancy, seeks to bring a precision medicine approach into vaccine practice by utilizing advanced genomic, epigenetic and bio-statistical approaches to better identify individuals susceptible to an adverse vaccine outcome to prevent or minimize adverse consequences. This is important because, as the CDC emphasizes, vaccines are generally given to healthy persons preventatively, and because of their widespread use, any safety issue, even if rare, can impact large numbers of people. The results of this study, while preliminary, suggest that we currently underestimate the group susceptible to an adverse vaccine effect.
We found a 6-fold increased risk of autoimmune disease in the group exposed to vaccines.
Certain vaccines, or adjuvants, have been implicated in autoimmune conditions such as thrombocytopenic purpura, rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis and Guillain-Barre syndrome. The spectrum of autoimmunity encompasses around 80 disorders, most considered rare, but combined have an estimated population prevalence of 4.5 percent to 9.4 percent. While pathogenic mechanisms of autoimmune disease are not well understood overall, and even less so with autoimmune sequelae following vaccination, contemporary thinking favors environmental factors triggering autoimmunity in genetically-susceptible individuals, involving epigenetic regulation.
Proposed mechanisms by which vaccines may contribute to autoimmune reactions are molecular mimicry (structural similarity between a vaccine component and self-antigen) and bystander activation (microbial agents activate pre-primed autoreactive immune cells).
Some studies have found that vaccination and atopic disorders, such as asthma, eczema and other allergies, are associated, while others have not.
Childhood infections appear to provide significant protection from atopy and it has been suggested that vaccination can contribute to atopy by inducing an imbalance between the two classes of T helper cells (Th1 and Th2) in genetically-susceptible individuals.
We found an over 4-fold increased risk of asthma and over 6-fold risk of asthma attack in those exposed to vaccination. This finding is consistent with Odent et al which found receiving DTP vaccine, versus no receipt, was associated with increased risk of asthma, Risk Ratio 5.43, Confidence Interval 1.93 to 15.30. In that study, over half of the group not receiving DTP were exposed to other vaccines and the group with the lowest prevalence of asthma were not exposed to any vaccine, 10.7 percent for DTP group versus 1.1 percent in group receiving no vaccines, though the latter’s small number limited statistical comparisons.
Most studies of vaccination and developmental outcomes evaluated MMR or thimerosol exposure and autism. These studies typically found no association, which is consistent with the results of this study, though the number of autism cases in this study was small. The few studies that evaluate potential associations between vaccination and neurodevelopmental disorders beyond autism have typically used a small dataset of neuropsychiatric evaluations at 7 to 10 years from the nineteen nineties in which all participants received all first-year vaccines.
Studies using this dataset have produced conflicting results.
A recent pilot study using claims data found a temporal relationship between vaccination and onset of certain neuropsychiatric disorders.
While contributors to the rise of developmental disability in children from 9.5 percent in 2009 to 16.9 percent has been grossly understudied, current thinking favors multiple contributors, including the immune system which is essential to normal brain development and is implicated in the pathogenesis of several neurodevelopmental disorders. Epigenetic research is exploring the complex relationship between developmentally-regulated genetic expression and interplay of prenatal and childhood environmental risk factors and exposures, in addition to factors such as socioeconomic status, preterm-birth, and birthweight.
A study by Iqbal et al did not find an association between the number of vaccine antigens and neuropsychological outcomes.
However, a recent study examined the feasibility of examining nonantigen vaccine ingredients and found that out of 34 ingredients, only aluminum exposure could be consistently quantified, but did not subsequently evaluate aluminum’s impact on clinically meaningful outcomes. We found a strong association between vaccine exposure (versus no exposure) and development of a neurodevelopmental disorder, Hazard Ratio 5.84, Confidence Interval 3.02 to 11.27, even after controlling for gender, race, birth-weight prematurity, and other factors. This increased risk was primarily driven by speech disorders, developmental delays, tics, ADHD, and behavioral and motor disabilities.
The etiology of this association is unclear, but it suggests that vaccination may serve as an environmental influence in susceptible children.
Strengths of this Study.
Major strengths of this study are that it evaluated a captured population, enrolled a consecutive birth cohort, evaluated subjects only while enrolled, only relied upon medical records to determine diagnoses, encounters and vaccines administered, unlike prior works which often relied upon parental recall and survey data, had a completely unexposed cohort, and utilized groupings of health conditions, which can reveal relationships that are not apparent when evaluating specific disorders individually, particularly if they are rare.
Though some results were unexpected, others are consistent with conclusions from prior systematic reviews, including by the IOM, such as the accepted causal relationship between vaccination and anaphylaxis, which we observed, or the rejection of a causal relationship between vaccination and cancer or MMR vaccine and autism. This contributes to the internal validity of this study’s findings.
This study also minimized the risk of misclassifying vaccine exposure. First, studies have shown good agreement between electronic vaccination and health records and both parental recall and manual medical record review, particularly for those unexposed to vaccines. Second, each subject’s HER contained vaccine administration data from HFHS and the state immunization registry, ensuring full capture of vaccinations. In Michigan, all providers are required to report vaccinations to the state registry within 72 hours of administration. This study, to our knowledge, includes the largest cohort of children completely unexposed to vaccination with observation in some subjects up to 18 years.
Limitations of this Study.
This study has limitations. As it is retrospective, we cannot exclude the possibility of unidentified confounders. However, this concern is tempered by the finding of significant associations between vaccination and particular outcomes, with some hazard ratios in the 2.5 to 6 times risk.
We lacked information on socioeconomic status, or potentially relevant post birth factors, such as diet or lifestyle, but did adjust for several important baseline confounders such as gender, ethnicity, gestational age and birthweight. To detect the potential for uncontrolled confounding, the literature suggests evaluating disorders with no expected causal association with vaccination, a control outcome, such as injuries or cancer. Importantly in this regard we found no association between vaccine exposure and cancer. Additionally, we relied on diagnosis codes in administrative data, which is commonly used in epidemiologic research but has some inherent limitations.
Unvaccinated children have less healthcare utilization overall.
Well visits coincide with the vaccination schedule and provide more opportunities for assessment and diagnosis in those receiving vaccines, compared to unvaccinated children, which could introduce an ascertainment bias. In this study, exposed children had an average of 7 annual encounters, Incidence Rate Ratio respective of having a chronic health condition.
Unexposed children had an average of 2 annual encounters but an average of almost 5 annual encounters if diagnosed with a chronic health condition. This likely demonstrates that when a child had a medical condition, parents sought healthcare. In fact, many conditions evaluated in this study are serious and cannot be self-treated, such as asthma, diabetes, anaphylaxis or asthma attack, warranting urgent medical attention. We nonetheless conducted several sensitivity analyses to explore the influence of healthcare utilization in order to improve the internal validity of this study and minimize potential ascertainment bias.
To ensure the unexposed group’s shorter follow-up duration did not influence the results, we repeated the Cox proportional hazards analysis for the chronic health composite outcome for those in the plan for one, three and five years and for those who had at least one healthcare encounter, which demonstrated results consistent with the overall findings. The association between vaccination and developing a chronic health condition was independent of these factors. Therefore, our findings do not appear to be due to differential use of health resources.
Our study solely evaluated whether or not vaccination was associated with clinically relevant outcomes, conditions that currently contribute to the rising chronic health disease burden in children. We did not evaluate the influence of temporal relationships, individual vaccines, or the number of vaccines, which limits this investigation but also minimizes the potential for reverse causality.
Conclusion.
In this study, we found vaccine exposure in children was associated with an increased risk of developing a chronic health disorder. This association was primarily driven by increased risk for asthma, atopy, eczema, autoimmune disease and neurodevelopmental disorders. This suggests that in certain susceptible children, exposure to vaccination may increase the likelihood of developing a chronic health condition, particularly for one of these conditions. Our preliminary findings cannot prove causality and warrant further investigation.
FIGURES AND TABLES.
Table 1. Birth Characteristics and Demographics Stratified by Vaccine Exposure Status.
Demographics.
For vaccinated and non-vaccinated, see original text.
Table 2. Incidence of Chronic Health Conditions Stratified by Vaccine Exposure Status.
Outcomes for Any vaccine exposure, and no vaccine exposure.
Table 3. Cox Proportional Hazards Regression Analysis for Vaccine Exposure and Development of a Chronic Health Condition.
Outcome, Unadjusted Hazard Ratio, and Adjusted Hazard Ratio, with a p 5 percent confidence interval.
Figure 1. Kaplan Meier Curve: 10-year Chronic Disease-Free Survival by Vaccine Exposure.
Index of Other Science Articles:
https://rumble.com/v3t4yzj-index-of-science.-music-by-dan-vasc.html
-
 19:16
19:16
Jasmin Laine
15 hours agoCBC Gets FACT-CHECKED By Guest—Carney BEGS Poilievre For Help
10.1K10 -
 8:50
8:50
The Shannon Joy Show
13 hours agoBREAKTHROUGH Cancer Treatments With Dr. Makis
2.96K2 -
 9:10
9:10
Faith Frontline
12 hours agoMatthew McConaughey Just Said What No Celebrity Dares to About Jesus
3.46K2 -
 27:03
27:03
Take FiVe - His Glory
1 day agoEp 2112: Sam Anthony: How Citizen Journalism is Replacing Legacy Media | Take Five
9.79K2 -
 10:01
10:01
Breaking Points
18 hours agoKJP GASLIGHTS On Biden's Age In BONKERS Book Tour
5.66K1 -
 11:31
11:31
Nate The Lawyer
16 hours ago $0.95 earnedJohn Bolton Indictment Explained | Even MSNBC Says He Is in BIG Trouble!
11.4K2 -
 25:46
25:46
DeVory Darkins
1 day ago $12.19 earnedICE raid erupts into chaos when protestors targeted ICE Agents as ABC suffers disastrous interview
20.7K30 -
 6:06
6:06
Congressman Eli Crane
20 hours agoThe "Affordable" Care Act | Democrats' Greatest Lies – Vol. 3
6.87K3 -
 1:07:05
1:07:05
TruthStream with Joe and Scott
1 day agoMorocco, Fix The World Project, EMF Protection, Camels and more! Premiers 10/22 All links below!! #502 Premiers 10/22 3pm pacific 6pm Eastern
81.3K12 -
 1:41:55
1:41:55
MattMorseTV
1 day ago $30.60 earned🔴Trump meets with GOP Senators over SHUTDOWN. 🔴
35.2K64