Premium Only Content
Revisiting Polio: Have We Been Misled About the Polio Vaccine’s Impact?
**Introduction: The Polio Narrative Under Scrutiny**
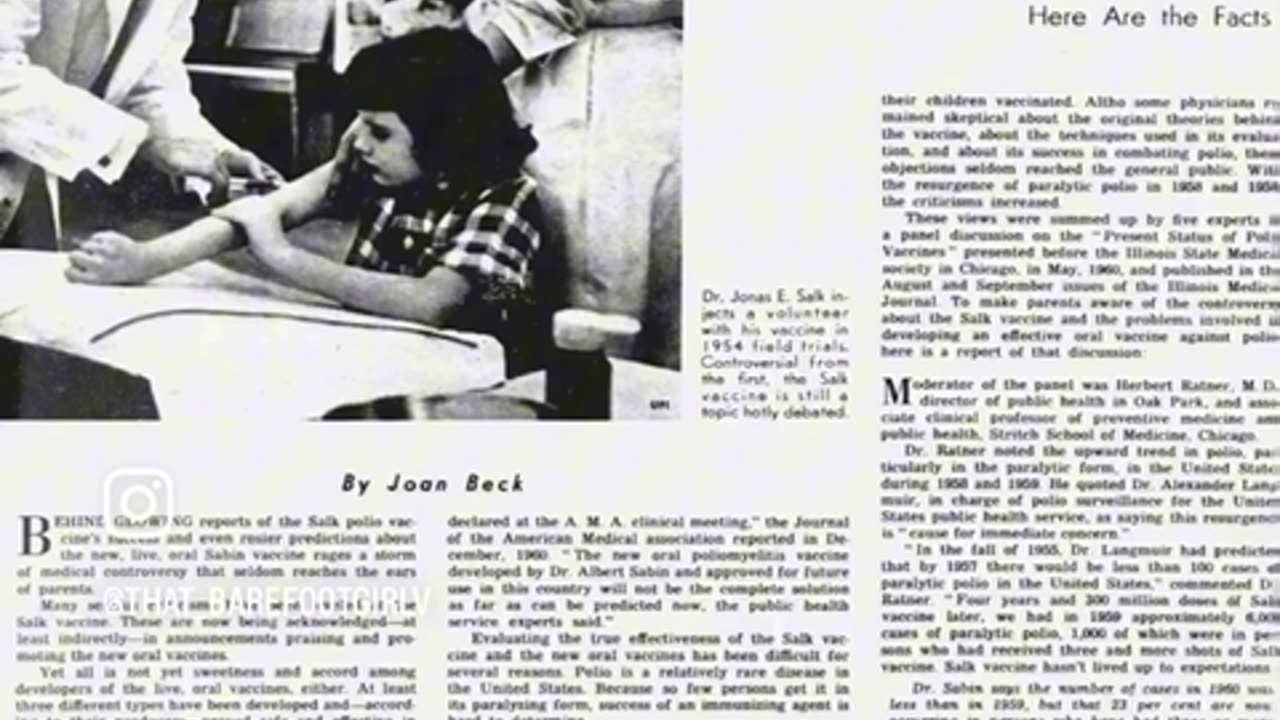
Polio, a word that has haunted the minds of generations, evokes images of iron lungs, paralyzed limbs, and widespread fear. The polio vaccine, introduced in the 1950s, is hailed as one of the greatest triumphs of modern medicine. However, recent analysis and historical records suggest that the narrative surrounding polio and the vaccine may not be as straightforward as we’ve been led to believe. Could it be that changes in diagnostic criteria and statistical adjustments played a significant role in the perceived success of the polio vaccine? Let’s take a closer look.
**A Glimpse Into the Past: Polio Before the Vaccine**
Before the introduction of the polio vaccine, the term "polio" was used broadly to describe various forms of paralysis, even when the paralysis was caused by viruses other than the poliovirus. For example, cases of viral meningitis, coxsackievirus, and echovirus, which can cause symptoms similar to those of polio, were often logged as polio cases. This broad classification inflated the number of polio cases, creating the impression of a widespread epidemic.
This is a critical point to consider. The viruses that caused polio-like symptoms still exist today, yet they no longer fall under the "polio" classification. This raises the question: how many of the cases recorded as polio before the vaccine was introduced were truly caused by the poliovirus?
**The Vaccine's Introduction and Changing Diagnostic Standards**
The introduction of the polio vaccine is often credited with drastically reducing the number of polio cases. However, what is frequently overlooked is the change in diagnostic criteria that occurred simultaneously. Before the vaccine, any case of temporary paralysis was often labeled as polio. However, after the vaccine’s introduction, only cases of paralysis lasting over 60 days were classified as polio. This change in the criteria naturally led to a significant drop in reported polio cases, as many cases that would have been counted as polio in the past were now excluded from the statistics.
This shift in diagnostic standards played a pivotal role in the apparent decline of polio cases post-vaccine. Rather than reflecting an actual reduction in the incidence of the disease, the decrease in reported cases may have been largely a result of redefined criteria rather than the vaccine's effectiveness itself.
**Redefining Epidemics: The Numbers Game**
In addition to changing diagnostic criteria, the definition of what constituted a "polio epidemic" was also altered. Before the vaccine, a polio epidemic was defined as 20 cases per 100,000 people. After the vaccine was introduced, the threshold for labeling an outbreak as an epidemic was raised to 35 cases per 100,000. This statistical adjustment further contributed to the perception that the vaccine was reducing the incidence of polio when, in reality, the change in numbers was partially due to altered definitions.
An article from the *Chicago Tribune* in 1960 highlighted these shifts, noting that the apparent reduction in polio cases and epidemics may have been more a reflection of changed definitions and diagnostic practices rather than an actual decrease in the disease's occurrence. By redefining what counted as polio and raising the bar for what was considered an epidemic, the medical community was able to present a narrative of success that may not have fully aligned with the reality.
**The Artificial Decline: Was It the Vaccine or the Redefinitions?**
The redefinition of polio and the recalibration of epidemic thresholds suggest that the reported decline in polio cases may not have been solely due to the vaccine’s efficacy. Instead, the numbers could have been significantly influenced by changes in how the disease was diagnosed and reported. By excluding polio-like illnesses and changing the criteria for what constituted a polio case, an artificial decrease in reported cases emerged, which medical authorities attributed to the vaccine's success.
This revelation invites us to reconsider the narrative we've been told. While the polio vaccine may have had a positive impact, the extent of its effectiveness may have been exaggerated by the concurrent changes in diagnostic and reporting practices. The implications of this are profound, as it suggests that the public's understanding of the vaccine's success may be based on manipulated data rather than a true reflection of its impact.
**Conclusion: A Call for Deeper Inquiry and Transparency**
The history of polio and its vaccine is a complex one, and it is essential that we approach it with a critical eye. The changes in diagnostic criteria, the redefinition of what constituted an epidemic, and the exclusion of polio-like illnesses from the statistics all point to the possibility that the narrative of the vaccine’s success may have been crafted as much by statistical manipulation as by medical achievement.
As we continue to place our trust in vaccines and other medical interventions, it is crucial that we demand transparency and honesty from medical authorities. The story of polio serves as a reminder that numbers can be manipulated, and that the truth can sometimes be obscured by changes in definitions and criteria. Only by asking the right questions and digging deeper into the data can we ensure that we are truly informed about the medical history that shapes our lives.
-
 2:45
2:45
FragmentsOfTruth
3 days agoTHE MONSTER STUDY
221 -
 3:11:52
3:11:52
Esports Awards
4 hours agoEsports Awards: Decade Awards 2025
41.2K3 -
 1:02:58
1:02:58
Sarah Westall
2 hours agoMILITARY WHISTLEBLOWER: How Social Media Military Level Psyops are Manipulating You w/ Patrick Bergy
6.03K1 -
 30:41
30:41
Stephen Gardner
1 hour ago🔥WHITE HOUSE GETS UNEXPECTED BIG WIN!
4.17K10 -
 9:39
9:39
MattMorseTV
3 hours ago $0.31 earnedVance just DROPPED a BOMBSHELL.
10.4K36 -
 2:40:14
2:40:14
DooM49
3 hours agoThe Grind for Battlefield 6 Skins - A-10 Unlocked
258 -
 1:47:49
1:47:49
Jeff Ahern
4 hours ago $0.31 earnedThe Sunday Show!
120K4 -
 LIVE
LIVE
Spartan
2 hours agoExpedition 33, Halo Later on (Maybe)
49 watching -
 LIVE
LIVE
Meisters of Madness
1 hour agoFinals and Wuchang!
55 watching -
 LIVE
LIVE
Lofi Girl
2 years agoSynthwave Radio 🌌 - beats to chill/game to
215 watching