Premium Only Content
Brachytherapy: Treatment of vaginal cancer
Treating Womb Cancer with Intrauterine Radiation:
Introduction
Womb cancer, also known as endometrial cancer, is a type of cancer that begins in the lining of the uterus. It primarily affects postmenopausal women but can occur in younger women as well. While surgery is often the first line of treatment, intrauterine radiation therapy, or brachytherapy, is a vital component in the comprehensive management of this disease. This article delves into the mechanisms, benefits, and considerations of treating womb cancer with intrauterine radiation.
Understanding Intrauterine Radiation
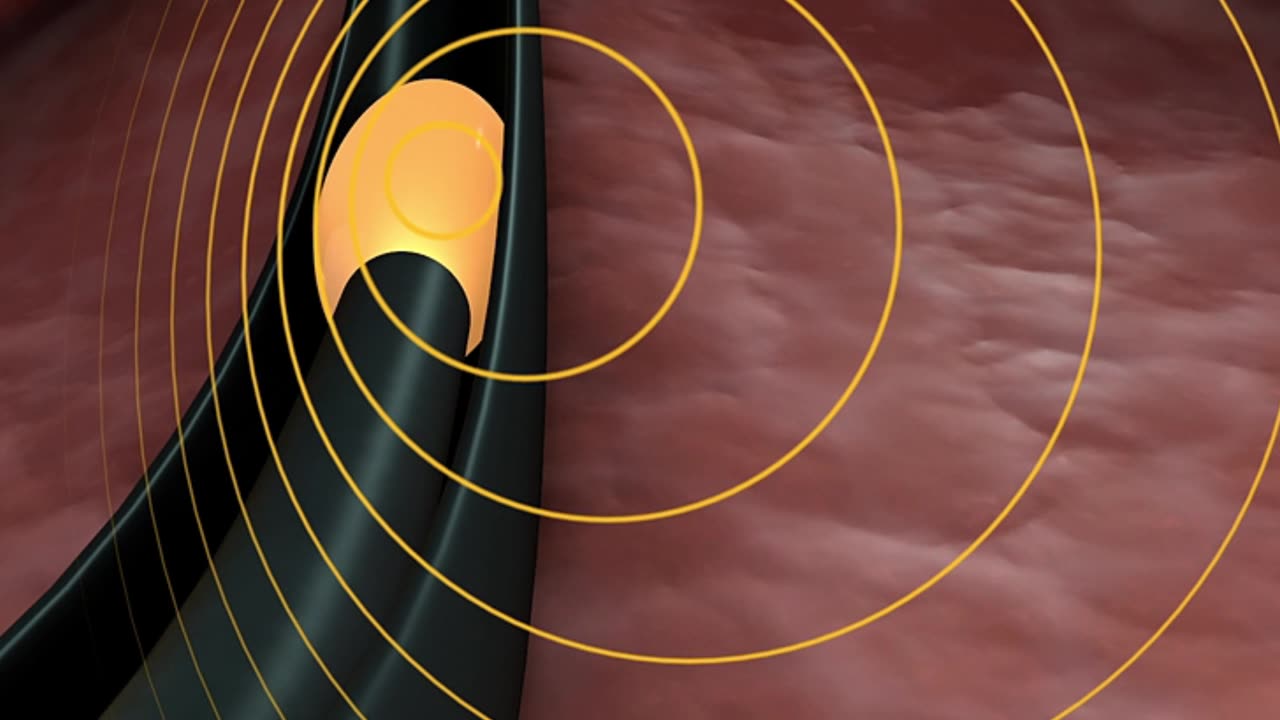
Intrauterine radiation therapy involves placing a radioactive source directly within the uterus. This method allows a high radiation dose to be delivered precisely to the tumour site while minimizing exposure to surrounding healthy tissues. Brachytherapy is typically used after surgery to destroy any remaining cancer cells, thereby reducing the risk of recurrence.
Mechanisms of Action
The procedure usually involves the insertion of a device called an applicator, into the uterus. This applicator serves as a conduit for the radioactive material. The treatment can be categorized into two main types based on the duration of radiation exposure:
High-Dose Rate (HDR) Brachytherapy: Involves delivering a high dose of radiation over a short period, typically in a series of outpatient sessions. Each session lasts only a few minutes.
Low-Dose Rate (LDR) Brachytherapy involves a continuous low dose of radiation over a longer period, often requiring an overnight hospital stay.
Procedure
The process of intrauterine radiation therapy involves several steps:
Preparation: The patient undergoes imaging studies, such as MRI or CT scans, to determine the exact location and size of the tumour. This aids in the precise placement of the applicator.
Insertion: Under anesthesia, the applicator is inserted into the uterus. The position is confirmed using imaging techniques to ensure accurate delivery of radiation.
Radiation Delivery: Depending on whether HDR or LDR brachytherapy is used, the radioactive source is placed within the applicator for the designated period.
Removal: After the treatment duration, the applicator is carefully removed, and the patient is monitored for immediate side effects.
Benefits of Intrauterine Radiation
Targeted Treatment: Direct delivery of radiation to the tumour site enhances the effectiveness of the treatment while protecting surrounding healthy tissue.
Reduced Side Effects: Compared to external beam radiation, brachytherapy often results in fewer side effects, such as damage to the bladder or rectum.
Shorter Treatment Time: HDR brachytherapy, in particular, offers the advantage of shorter overall treatment times, which can be more convenient for patients.
Improved Outcomes: Studies have shown that combining surgery and intrauterine radiation can significantly improve survival rates and reduce the risk of cancer recurrence.
Considerations and Side Effects
While intrauterine radiation is generally well-tolerated, it is not without potential side effects. Patients may experience:
Vaginal Discharge: Temporary increase in discharge or bleeding.
Fatigue: Common during and after treatment.
Bladder and Bowel Changes: Irritation can lead to urinary frequency or diarrhea.
Vaginal Stenosis: Narrowing of the vaginal canal, which can affect sexual function.
To mitigate these side effects, healthcare providers offer supportive care and guidance throughout treatment.
Conclusion
Intrauterine radiation therapy is a pivotal treatment modality for womb cancer, offering targeted, effective, and relatively low-risk management of this condition. As part of a multimodal approach that includes surgery and possibly chemotherapy, brachytherapy enhances the chances of a successful outcome for patients with endometrial cancer. Ongoing research and advancements in radiation technology continue to improve the precision and efficacy of this treatment, providing hope and improved quality of life for those affected by womb cancer.
-
 1:20:41
1:20:41
TRAGIKxGHOST
2 hours agoTrying to get SCARED tonight! | Are You SCARED!? | Screams Beyond Midnight | Grab a Snack
6.17K2 -
 LIVE
LIVE
StuffCentral
3 hours agoI'm baaack (no you can't play with me.. unless you a healer)
110 watching -
 2:25:11
2:25:11
TheSaltyCracker
5 hours agoTrump Is Not Dead ReEEeStream 8-31-25
70.9K101 -
 3:09:16
3:09:16
THOUGHTCAST With Jeff D.
3 hours ago $0.67 earnedLabor Day Weekend FORTNITE With THOUGHTCAST Jeff & the squad
11.7K4 -
 3:44:05
3:44:05
Rallied
6 hours ago $4.00 earnedSolo Challenges All Day
40.5K1 -
 LIVE
LIVE
iCheapshot
6 hours ago $0.20 earnedCall of Duty: Black Ops Campaign
44 watching -
 4:39:16
4:39:16
Meisters of Madness
7 hours agoMadness in a Pod
7.59K1 -
 1:25:44
1:25:44
HELMETFIRE
3 hours ago🟢GAMING WITH FIRE EP9🟢
7.91K -
 1:24:08
1:24:08
Jean-Claude@BeyondMystic
15 hours ago🌀 THE WACKY WOO SHOW 3I ATLAS ALIEN INVASION with DICK ALLGIRE & JC - AUG 31 , 20254
47.4K62 -
 2:26:21
2:26:21
vivafrei
14 hours agoEp. 279: Patel's GF Sues for Defamation! Rogue Judges vs. Trump! Raja Jackson, Kick Stream & MORE!
143K81