Premium Only Content
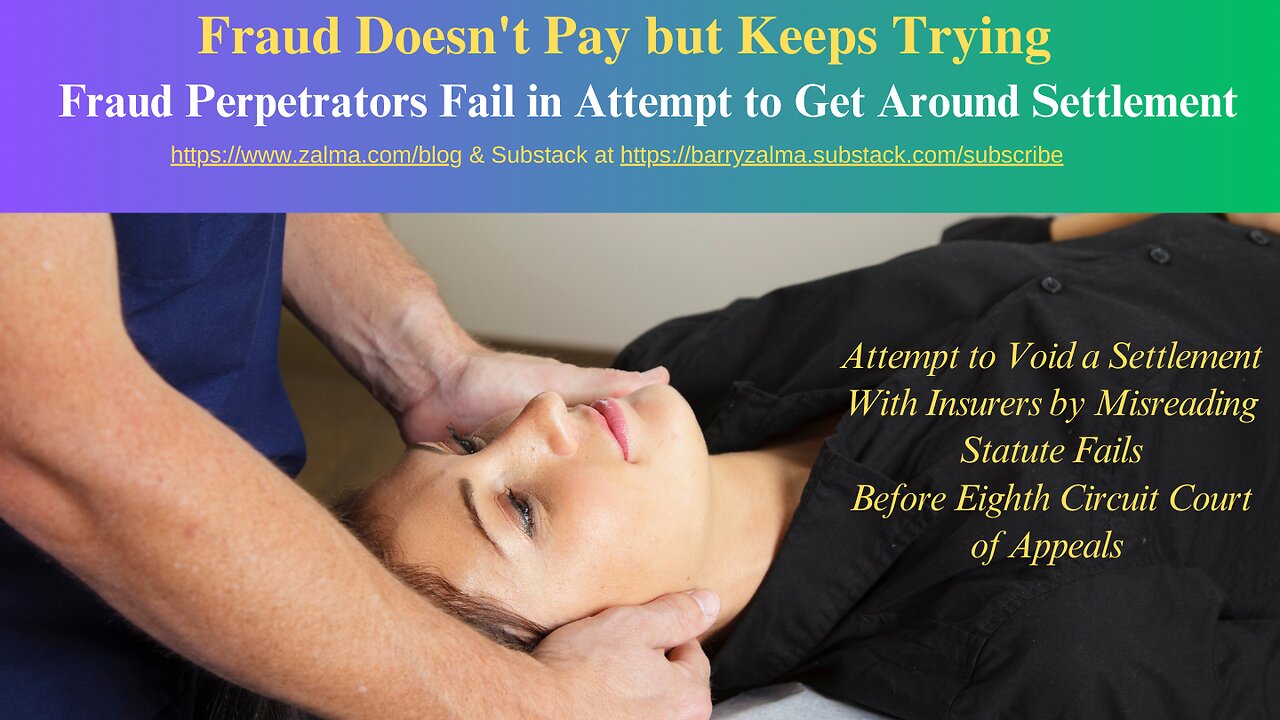
Fraud Doesn't Pay but Keeps Trying
Fraud Perpetrators Fail in Attempt to Get Around Settlement
Post 4849
"Operation Back Cracker" (a joint state and federal criminal investigation) exposed a ring of Minnesota healthcare providers (mostly chiropractors) who were recruiting car accident victims and fraudulently billing auto insurers for their treatment. In related civil settlements, several providers agreed not to bill some of the insurance companies for any treatment provided to their insureds.
The settlement agreements reduced the ability of the fraudulent chiropractors who entered into the settlement agreements to profit from fraud against the insurers who settled. The chiropractors sued seeking to void the no-bill agreements used to reduce the insurers losses, by claiming the settlements violated the Minnesota No-Fault Automobile Insurance Act. The district court enjoined Illinois Farmers Insurance Company and others (together, Farmers) from entering into or enforcing the no bill agreements.
In Taqueria El Primo LLC, et al v. Illinois Farmers Insurance Company; et al Coalition Against Insurance Fraud Amicus, No. 23-3128, United States Court of Appeals, Eighth Circuit (July 31, 2024) in a question of first impression: whether no-bill agreements "ha[ve] the effect of providing[] managed care services" or place "preestablished limitations on [medical expense] benefits" within the meaning of the No-Fault Act and the Eighth Circuit resolved the issue.
THE LITIGATION
Plaintiffs represent both an injunctive class and a damages class of people insured by Farmers. They sued after discovering that Farmers has confidential nobill agreements with a few providers, alleging that the agreements violate the NoFault Act.
The No-Fault Act requires insurers to provide "[b]asic economic loss benefits" when an insured is injured by the maintenance or use of a motor vehicle. Those benefits provide reimbursement for all loss suffered through injury including income loss, replacement services loss, and medical expense.
The no-bill agreements prevent providers from submitting bills to Farmers or its insureds. In a typical agreement, the provider "agrees not to submit, cause to be submitted, or seek payment on any Farmers claim . . . for any services performed from" the date of the settlement to a specified date-sometimes "into perpetuity."
Some agreements go so far as to clarify that bills submitted by the provider are void and that the provider "may not collect the bills from Farmers and/or the insured/claimant who received the treatments."
ANALYSIS
The No-Fault Act does not create a private right of action, so Plaintiffs sought an injunction under the Uniform Deceptive Trade Practices Act and damages under the Consumer Fraud Act. The district court granted summary judgment to the injunctive class and enjoined Farmers from entering into or enforcing no-bill agreements. It ruled that the no-bill agreements "ha[ve] the effect of providing[] managed care services" and set "preestablished limitations on [medical expense] benefits"-both violations of the No-Fault Act. And that meant Farmers was, in turn, violating the UDTPA by certifying that its policies complied with the No-Fault Act when they did not.
The district court thought that Farmers "reverse-engineered managed care services" by creating a program where "[t]he effect is the same: insureds may only receive services from a subset of providers that Farmers has decided to favor over others." This conclusion unmoored "the effect of" from its context.
The phrase "or has the effect of providing" broadens the means ("provides"), not the ends ("managed care services"). The alleged program must be one that uses health care providers managed, owned, employed by, or under contract with a health plan company. The no-bill providers, who make up a miniscule portion of Minnesota providers, are the only ones under contract with Farmers. And the program excludes, rather than uses, them. This does not fit subdivision 1(c)'s express definition of a "managed care services" program.
If a no-bill provider complies with its agreement and never bills Farmers or its insured, the insured never incurs a medical expense. An insurer violates the No-Fault Act if it refuses to reimburse an insured who has incurred a qualifying expense. But an insurer does not violate the Act by enforcing a no-bill agreement against a provider.
Because the injunction prohibits the latter, it cannot stand and the injunction was vacated.
ZALMA OPINION
The chiropractors entered into a settlement to avoid losses as a result of being caught defrauding insurers. By promising not to bill the insurers for the future the insurers recouped their losses and incurred no new fraudulent losses. Attempting to break away from the agreement and continue to defraud the insurers they sought an injunction against enforcing the deal. The USDC fell for the claim and the Eighth Circuit saw through the scheme and vacated the injunction proving to Farmers and the other insurers involved you can't trust fraudsters.
(c) 2024 Barry Zalma & ClaimSchool, Inc.
Please tell your friends and colleagues about this blog and the videos and let them subscribe to the blog and the videos.
Subscribe to my substack at https://barryzalma.substack.com/subscribe
Go to X @bzalma; Go to Newsbreak.com https://www.newsbreak.com/@c/1653419?s=01; Go to Barry Zalma videos at Rumble.com at https://rumble.com/account/content?type=all; Go to Barry Zalma on YouTube- https://www.youtube.com/channel/UCysiZklEtxZsSF9DfC0Expg
Go to the Insurance Claims Library – https://lnkd.in/gw
-
 2:08:03
2:08:03
Barry Cunningham
3 hours agoBREAKING NEWS: PRESIDENT TRUMP SPEAKS TO MCDONALD'S EXECUTIVES AND MORE NEWS!
20.8K16 -
 LIVE
LIVE
Spartan
4 hours agoPro Halo Player, insta locking Neon, plays Valorant for the first time since Beta. Rusty af on MnK
130 watching -
 0:54
0:54
Gaming on Rumble
6 hours agoRumble Premium x Preplexity Pro Subscription Bundle
2.26K1 -
 LIVE
LIVE
LFA TV
1 day agoLIVE & BREAKING NEWS! | MONDAY 11/17/25
550 watching -
 LIVE
LIVE
Sen D Regon
1 hour agoExophobia Ep1 | Shoot'en Me Some Space Aliens
23 watching -
 LIVE
LIVE
JDubGameN
2 hours agoArc Raiders | Road to 100 Followers | DubNation LIVE
26 watching -
 LIVE
LIVE
The Jimmy Dore Show
3 hours agoWill Trump’s Attacks on Massie & MTG KILL MAGA? Candace SILENCES Zionist CNN Reporter! w/ Kim Bright
6,164 watching -
 LIVE
LIVE
AUXgaming
2 hours ago👽 Charles and Lewis need to give the BIRD to their Boss! 👽 #1 ALIEN ON RUMBLE 👽 POSITIVE VIBES! 👽
30 watching -
 53:42
53:42
The White House
9 hours agoPresident Trump Delivers Remarks at McDonald's Impact Summit
18.9K18 -
 44:39
44:39
Donald Trump Jr.
3 hours agoBuilders vs Bureaucrats, LIVE News Coverage | TRIGGERED Ep.292
87.9K69