Premium Only Content
Current diagnosis and management of erectile dysfunction. A Puke (TM) Audiopaper.
Current diagnosis and management of erectile dysfunction.
A Narrative review.
Christopher G McMahon.
cmcmahon@acsh.com.au
doi: 10.5694/mja2.50167
https://www.mja.com.au/system/files/issues/210_10/mja250167.pdf
Index of Other Science Articles:
https://rumble.com/v3t4yzj-index-of-science.-music-by-dan-vasc.html
Summary.
Erectile dysfunction (“E-D”) is a common male sexual dysfunction associated with a reduced quality of life for patients and their partners.
ED is associated with increasing age, depression, obesity, lack of exercise, diabetes mellitus, hypertension, dyslipidaemia, cardiovascular disease and lower urinary tract symptoms related to benign prostatic hyperplasia.
The evaluation of men with “E-D” requires a full medical and personally and culturally sensitive sexual history, a focused clinical examination, fasting glucose levels, a fasting lipid profile and, in select cases, a total testosterone level and a prostate-specific antigen test.
Treatment of “E-D” requires lifestyle modification, reduction of comorbid vascular risk factors, and treatment of organic or psychosexual dysfunction with either pharmacotherapy alone or in combination with psychosexual therapy.
Between 60 percent and 65 percent of men with “E-D”, including those with hypertension, diabetes mellitus, spinal cord injury and other comorbid medical conditions, can successfully complete intercourse in response to the phosphodiesterase type 5 inhibitors (PDE5i) sildenafil, tadalafil, vardenafil and avanafil.
Patient-administered intracorporal injection therapy using vasodilator drugs such as alprostadil is an effective treatment and is useful in men who fail to respond to oral pharmacological agents.
Surgical treatment of “E-D” with multicomponent inflatable penile implants is associated with high satisfaction rates.
Penile arterial revascularisation and venous ligation surgery are associated with relatively poor outcome results in men with penile atherosclerotic disease or corporal veno-occlusive dysfunction.
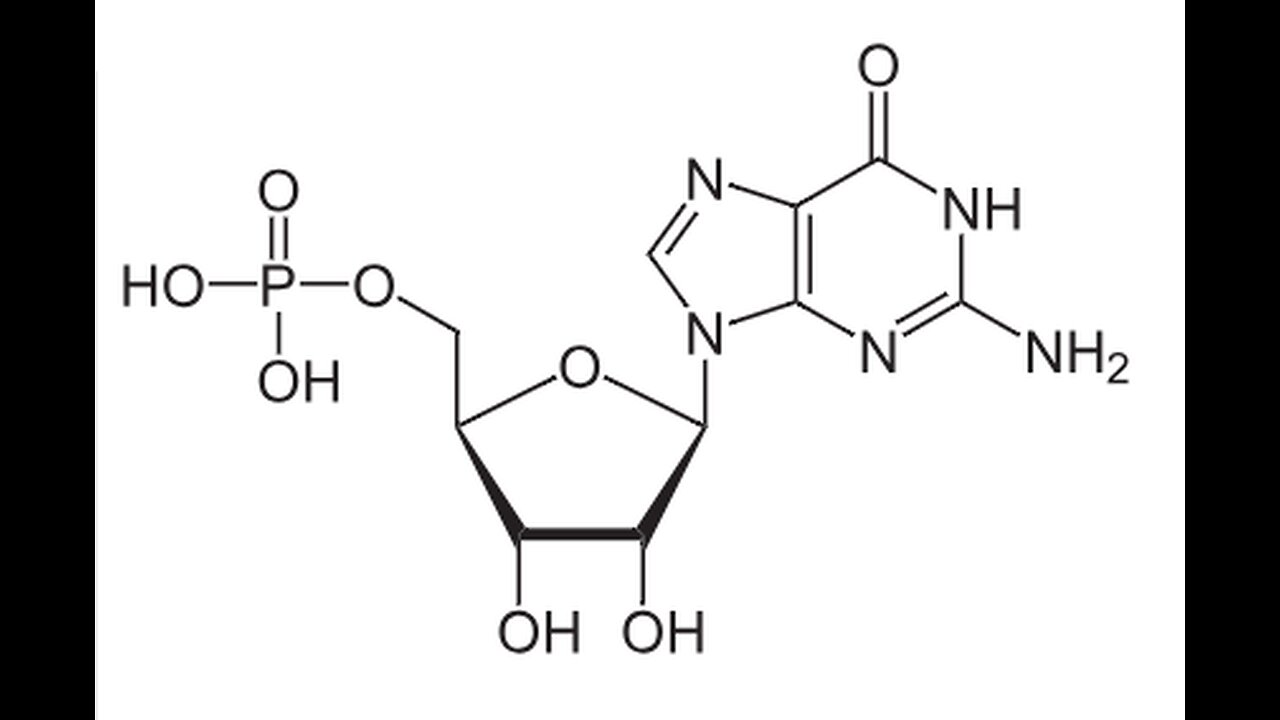
Erectile dysfunction (“E-D”) is a common male sexual dysfunction associated with a reduced quality of life for patients and their partners. Definitions of “E-D” have been proposed by the National Institutes of Health Consensus Development Conference Statement in 1992, the American Psychiatric Association’s Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5), text revision, and the World Health Organization’s International Classification of Diseases, tenth edition (ICD-10). The most commonly quoted definition of “E-D” from the National Institutes of Health is the inability to get or keep an erection firm enough for satisfactory sexual intercourse. Penile erection is a neurovascular phenomenon that requires dilation of penile vasculature, relaxation of corporal smooth muscle, increased intracavernosal blood flow and a normal veno-occlusive function. Eighty per cent of “E-D” cases are due to penile vascular disease caused by endothelial dysfunction related abnormalities of the nitric oxide, cyclic guanosine 3 5 monophosphate (NO-cGMP) system.
“E-D” may be an early manifestation of generalised endothelial dysfunction and a predictor and a precursor of other forms of cardiovascular disease. Epidemiological data from Australian, American and British observational studies estimate the prevalence of complete “E-D” as about 5 percent among 40-year-old men, 10 percent among men in their sixties, 15 percent among men in their seventies and 30 to 40 percent among men in their eighties. Prevalence studies show that, when controlling for other factors, “E-D” is associated with increasing age, depression, obesity, lack of exercise, diabetes mellitus, hypertension, dyslipidaemia, cardiovascular disease, lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia.
The Multinational Survey on the Aging Male (MSAM-7) study reported that men with LUTS had an overall prevalence of “E-D” of 49 percent, complete erectile failure in 10 percent, and an overall prevalence of ejaculatory disorders of 46 percent. Antihypertensive and antidepressants drugs may cause “E-D” as an adverse drug reaction and their discontinuation does not always result in the recovery of erectile function. Thiazide diuretics, non-selective alpha-blockers, and beta2-blockers may cause “E-D”, but angiotensin-converting enzyme inhibitors, calcium channel blockers, alpha1-blockers and angiotensin receptor blockers have a low risk of ED. Even though the incidence of “E-D” rises significantly with increasing age, studies indicate that 55 to 70 percent of men aged 77 to 79 years are sexually active. However, only half of the men who self-report “E-D” are concerned about it. This narrative review analyses selected published peer reviewed “E-D” practice guidelines. The PubMed electronic database from 2008 to 6 February 2018, the United States Food and Drug Administration website, the European Medicines Agency website and the websites of multiple national and regional urological and sexual medicine association and societies were searched for published guidelines. Search terms included the Medical Subject Headings (MeSH) “erectile dysfunction”, “impotence”, “guidelines” and “recommendations”.
The search terms and selection criteria were satisfied by 11 guidelines. Eight guidelines made recommendations on both the evaluation and treatment of ED. The remaining three guidelines were limited to hormonal evaluation, “E-D” pharmacotherapy and the surgical management of “E-D” and did not discuss patient evaluation. These guidelines were subject to critical assessment and were synthesised in an attempt to highlight areas of agreement and possible inconsistencies.
Evaluation of patients.
Each guideline proposed similar frameworks for the assessment of men seeking treatment for ED. All agreed that “E-D” can be an early symptom of diabetes mellitus or cardiovascular disease. A full medical and personally and culturally sensitive sexual history and thorough clinical examination of the patient are needed to:
Confirm that the patient has “E-D” and or other sexual dysfunctions, such as hypoactive desire or premature ejaculation.
Assess the onset, severity and duration of the condition and the impact on the patient’s partner.
Identify the presence and contribution of potentially reversible causes (medications, drug or alcohol misuse), risk factors, comorbid disease or psychosocial factors.
Determine whether the cause of “E-D” is psychogenic, organic (eg, vasculogenic, endocrine, neurological or end organ disease, such as penile deformity due to Peyronie disease) or mixed (Box 1); and
Assess the fitness of the patient for resuming sexual activity. Any relationship between anxiety and “E-D” should be explored.
Psychogenic “E-D” is likely in younger men with no vascular risk factors who report an abrupt onset of “E-D” and persistent early morning or nocturnal erections. The causes of psychogenic “E-D” are manifold and include sexual performance anxiety, global anxiety, relationship problems, depression, guilt and or fear. Careful enquiry should be made about current medications, such as thiazide diuretics, non-selective alpha-blockers, beta 2-blockers and antidepressants as well as the use of recreational drugs. Several patient self-administered validated questionnaires have been developed to objectively score the erectile function. The short five-question form of the International Index of Erectile Function (IIEF-5) and the Sexual Health Inventory for Men (SHIM) are useful for both diagnosis and assessment of response to treatment.
Physical examination.
A focused physical examination in men with “E-D” involves examination of general body habitus and genital anatomy and should identify any related abnormalities, for example, Peyronie plaques), endocrine signs and possible comorbidities (neurological, vascular, and possible life-threatening conditions). The presence, size and consistency of testes and adnexa are required to evaluate androgen status and the presence of atrophy or hypogonadism. A digital rectal examination is required in men over the age of 50 years or in men with an increased risk of prostate adenocarcinoma or LUTS suggesting benign prostatic hyperplasia.
Clinical investigations.
Laboratory investigations The need for clinical investigation depends on the patient’s history and examination findings.
The International Consultation on Sexual Medicine of the International Society for Sexual Medicine proposes that laboratory tests for men with “E-D” include fasting glucose level, fasting lipid profile and, in select cases, total testosterone level. The American Urological Association and most other guidelines recommend screening for prostate cancer in men seeking treatment for “E-D” with a digital rectal examination and prostate-specific antigen test in selected high risk patients or symptomatic patients with LUTS. Undiagnosed type 2 diabetes mellitus has been reported to occur in 5 to 12 percent of men with ED. Furthermore, “E-D” is reported to occur in 35 to 70 percent of men with type 2 diabetes mellitus. “E-D” occurs at an earlier age in men with type 2 diabetes mellitus compared with men without diabetes mellitus, and the age-adjusted probability of complete “E-D” is nearly three times higher. The presence of occult impaired glucose tolerance impaired fasting glucose or type 2 diabetes mellitus can be assessed with a fasting plasma glucose, 5.6 to 6.9 nano mole per liter or greater than or equal to 7.0 nano mole per Liter, respectively, and or glycated haemoglobin, greater than or equal to 5.7 percent or greater than or equal to 6.5 percent, respectively, and, if indicated, a 75 gram oral 2-hour glucose tolerance test.
There is a guideline consensus that screening for low testosterone with a morning total testosterone assay, eight to eleven AM, is the investigation of choice and is appropriate in men with “E-D” and hypoactive sexual desire, incomplete response to phosphodiesterase type 5 (PDE5) inhibitors (PDE5i), delayed ejaculation, and in all men with known diabetes mellitus.
The prevalence of low total testosterone levels in men with “E-D” varies widely across studies and ranges from 12.5 percent to 35 percent.
The threshold of testosterone to maintain an erection is low, less than 5.5 nano mole per liter, and “E-D” is usually a symptom of more severe cases of hypogonadism. If total testosterone level is greater than or equal to 12 Nano moles per Liter, 346 nanogram per deciliter, testosterone deficiency is unlikely. If total testosterone is less than 12 Nano moles per liter, 346 Nano gram per deciliter, a second morning venous blood sample drawn after an interval of at least one week, together with serum luteinising hormone and prolactin levels is required. Serum luteinising hormone measurement is essential to identify the subtype of testosterone deficiency, and is elevated in primary hypogonadism or reduced in secondary hypogonadism. Measurement of sex hormone binding globulin may be useful in older and obese men or men with liver cirrhosis, with chronic, suspicious symptoms and a borderline total testosterone level. Hyperprolactinaemia has a causal association with hypogonadotrophic (secondary) hypogonadism. Haemochromatosis has a causal association with hypergonadotrophic (primary) hypogonadism. Further investigations may be indicated based on history, examination findings and the results of these initial investigations and may include thyroid-stimulating hormone and other pituitary hormone levels, pituitary imaging studies chromosome analysis, full blood count, and urinalysis.
Specialized testing.
All guidelines agree that most patients do not need further investigations unless specifically indicated. Indications for the following specialised investigations include:
Patients who wish to know the aetiology of their Eoung patients with lifelong ED.
Patients with a history of pelvic, perineal or genital trauma.
Patients with an abnormality of the testes or penis found on examination; and
Patients unresponsive to medical therapies who may desire surgical treatment for ED.
Psychological assessment.
All guidelines agree that psychological assessment of men with “E-D” may provide information on the contribution of relationships, cultural and religious factors, depression and other psychological factors. Patients with comorbid psychiatric disorders or younger men with lifelong primary “E-D” should be referred to a psychiatrist or psychologist with an interest in sexual health.
Nocturnal penile tumescence and rigidity testing.
Nocturnal and early morning erections are normal physiological events and occur during rapid eye movement sleep. Reduced or absent nocturnal erections usually indicate organic ED. The presence, frequency, duration and rigidity of nocturnal erections can be measured with nocturnal penile tumescence and rigidity testing using a RigiScan monitor (TIMM Medical Technology).
However, nocturnal penile tumescence and rigidity testing is more of historical interest and its contemporary use in the evaluation of men with “E-D” is largely limited to medico-legal assessment of erectile function.
Intracavernous injection test.
This office test involves a physician-administered intracorporal injection of a vasoactive drug such as alprostadil and the assessment of penile rigidity or deformity after 10 minutes. The development of a rigid erection within 10 minutes that lasts for 30 minutes suggests psychogenic ED. However, its use as a diagnostic test is limited because a positive result can also be found in patients with mild vascular disease.
Vascular testing.
Several vascular tests exist, including colour duplex Doppler imaging, penile pharmacoangiography and dynamic infusion cavernosometry and cavernosography (DICC). Colour duplex Doppler imaging after an intracorporal injection of a vasoactive drug, for example alprostadil, provides information about penile haemodynamics and can distinguish arterial insufficiency and veno-occlusive dysfunction from other causes of ED. All guidelines agree that pharmacoangiography should be reserved for young men with arterial trauma and abnormal duplex haemodynamics or for embolisation of high flow priapism due to an arterio-lacunar fistula following penile or perineal trauma. DICC involves the perfusion of the corpora cavernosa with saline and a radio-opaque dye after an intracavernosal injection of a vasodilator drug to determine the efficacy of the veno-occlusive mechanism and the site of corporal venous leakage. These additional investigations, vascular reconstructive surgery and or venous ligation surgery are rarely conducted in the contemporary management of ED.
Neurophysiological testing.
Neurophysiological testing can indirectly measure the integrity of the perineal nerve by measurement of the sacral reflex arc latency and signal amplitude and has limited clinical utility.
Treatment options.
Treatment of “E-D” requires lifestyle modification to reduce the impact of comorbid vascular risk factors and treatment of organic or psychosexual dysfunction with either pharmacotherapy alone or in combination with psychosexual therapy. Its efficacy, benefits, appropriateness and risks should be discussed with patients and partners so their expectations are realistic. The treatment options for men with “E-D” are effective, safe and well tolerated (Box 2). Treatment selection depends on the severity and aetiology of “E-D”, the patient’s overall health and comorbid disease and the patient’s and their partner’s choice. Progression from first-line oral agents through second- and third-line therapies is indicated in treatment failures.
Management of patients with coronary artery disease.
“E-D” and coronary artery disease share the risk factors of dyslipidaemia, hypertension, smoking, diabetes, obesity, lack of physical activity and a familial history of early onset of coronary artery disease. “E-D” may be a predictor and a precursor of other forms of cardiovascular disease morbidity and mortality; it confers a 1.46-fold increased risk for cardiovascular disease. Men with proven or suspected vasculogenic “E-D” or multiple vascular risk factors, especially diabetes mellitus, should be screened for silent myocardial ischaemia with exercise electrocardiography, a coronary artery calcium score or coronary computed tomography angiography.
Most “E-D” guidelines follow the Second Princeton Consensus Panel guidelines for managing “E-D” in patients with cardiovascular disease and recommend assigning patients according to their risk factors to one of three risk levels: low, intermediate or high (Box 3). These risk categories can be used as the basis for a treatment decision for initiating or resuming sexual activity. Most men with coronary artery disease can safely resume sexual activity and undergo treatment for “E-D” following appropriate education and counselling. The cardiac risk of sexual activity in men with cardiovascular disease is minimal in properly assessed and advised patients. There is no evidence that currently approved “E-D” treatments add to the overall cardiovascular risk in patients with or without previously diagnosed cardiovascular disease.
Lifestyle changes and the modification of risk factors.
All guidelines agree that lifestyle changes and risk factor modification must precede or accompany any pharmacological or psychological “E-D” treatment. Lifestyle changes in men with comorbid cardiovascular or metabolic disorders, such as diabetes or hypertension, or psychosocial issues may achieve major clinical benefits. Cessation of smoking, maintaining ideal body weight, engaging in regular exercise and optimal management of these diseases may prevent the development of ED. In the Massachusetts Male Aging Study (MMAS), men who started physical activity in mid-life had a 70 percent reduced risk for “E-D” relative to those who remained sedentary, and regular exercise produced a significantly lower incidence of “E-D” over an 8-year follow-up period. Similarly, in a multicentre, randomised, open-label study of men with obesity, intensive exercise and weight loss significantly improved erectile function. Correction of dyslipidaemia may improve “E-D” within 3 months and significantly augment the response to “E-D” pharmacotherapy in unresponsive or refractory patients. However, there are conflicting data on the benefit of smoking cessation to improve erectile function.
Psychosexual therapy.
Psychosexual therapy for “E-D” is not standardised, as the foundation of anxiety varies between patients. Relationship difficulties, depression, guilt, previous sexual abuse, lack of sexual experience and problems with intimacy may all increase anxiety or conflict, which may then manifest as ED. Psychosexual treatments range from simple sex coaching and education through improved partner communication to cognitive and behavioural therapy and, in collaboration with the physician, are often combined with “E-D” pharmacotherapy. A large proportion of patients experience negative psychological consequences of organic “E-D”, which may result in progressively worsening performance anxiety and further deterioration of erectile function.
Oral pharmacotherapy.
Overall, 60 to 65 percent of men who have “E-D”, including those with hypertension, diabetes, spinal cord injury and other comorbid medical conditions, can successfully complete intercourse in response to the PDE5i sildenafil, tadalafil, vardenafil and avanafil (Box 4). PDE5i drugs selectively inhibit PDE5 isoenzyme, increasing the amount of cyclic guanosine monophosphate (cGMP) available for smooth muscle relaxation, and induce vasodilation, increased corporal blood flow and erection. The overall efficacy for the different PDE5i appears similar and is related to the severity of “E-D”, with significantly reduced efficacy in patients with severe vasculogenic “E-D”, diabetic “E-D” and post-radical prostatectomy. Sildenafil, tadalafil, vardenafil and avanafil have differing pharmacokinetic properties (Box 4). The patient’s and physician’s choice of PDE5i is based on cost, tolerability and pharmacokinetic properties, including speed of onset and duration of responsivity. The PDE5i drugs can be used long term, and although there is no clear evidence of tachyphylaxis or tolerance, users can become less responsive due to progressive worsening of underlying penile vascular disease. Most patients will prefer a trial of another PDE5i before proceeding to more invasive treatments. Daily dosing with tadalafil (2.5 milligrams, 5 milligrams or 10 milligrams) has similar efficacy and side effects rates to on-demand PDE5i, and is often selected as first-line treatment by men who engage in frequent intercourse or regard sexual intercourse spontaneity as a key treatment goal.
Daily dosing may improve endothelial function and improve or restore erectile function. Salvage of ondemand tadalafil failures, with high dose tadalafil (10 to 20 milligrams) administered daily or on alternate days, has been reported but is limited by the relatively high cost of treatment. PDE5i drug adverse effects are usually transient, mild to moderate in nature, dose dependent and often attenuate or disappear within 4 to 6 weeks of continued use. The most commonly reported adverse effects are headache (11 to 16 percent), facial flushing (2 to 11 percent), dyspepsia (4 to 10 percent), muscle or back pain (0 to 4 percent) and nasal congestion (2 to 9 percent). Non-arteritic ischaemic optic neuropathy (NAION) has been linked to PDE5i, although a causal relationship has not been established. In a population of 4 million veterans aged over 50 years with “E-D” treated with PDE5i, there was no increased risk for NAION (absolute risk, 4.6 cases per 10 000 men per year; relative risk, 1.02; 95 percent CI, 0.92 to 1.12). However, loss of vision or reduced vision requires urgent ophthalmological assessment and immediate cessation of PDE5i use. PDE5i drugs may exacerbate the hypotensive effects of aerosol, tablet or topical short- or long-acting organic nitrates, such as nitroglycerin or isosorbide dinitrate, and co-administration is contraindicated.
Intracorporal injection therapy.
Patient-administered intracorporal injection therapy using vasodilator drugs such as alprostadil is an effective treatment for “E-D” (Box 5). It is useful in men who fail to respond to oral pharmacological agents. Alprostadil resulted in an erection of sufficient rigidity for sexual intercourse in 72.6 percent of men with ED. The principal side effects of intracorporal injection of alprostadil are injection site pain in up to 30 percent of patients and corporal fibrosis resulting in the development of penile nodules and curvature in 9 to 23.3 percent of mid- and long term users. Priapism is a rare complication that can cause irreversible ischaemic damage and fibrosis of the corpora and permanent ED. Polyagent pharmacotherapy of alprostadil combined with other agents such as papaverine and or phentolamine is effective in 91.6 percent of patients, and appears effective as salvage therapy when treating patients with severe vasculogenic “E-D” unresponsive to oral pharmacotherapy. Intracorporal injection therapy combined with on-demand PDE5i has also been reported as effective salvage therapy and potentially allows lower drug doses and a reduced incidence of adverse effects. Relative contraindications to intracorporal injection therapy include anticoagulation, previous poor compliance and a history of priapism.
Vacuum constriction devices.
Vacuum constriction devices involve insertion of the flaccid penis into a vacuum cylinder and creation of a vacuum using an integrated hand or battery-operated vacuum pump to create marked tumescence or rigidity, which is maintained with a constricting ring at the base of the penis. A vacuum constriction device erection differs from a physiological erection because trabecular smooth muscle relaxation does not occur and blood is merely trapped within the corpora cavernosa distal to the constricting ring. Although 60 to 70 percent of men can eventually master the use of a vacuum constriction device and manage sexual intercourse, satisfaction rates vary considerably from as low as 27 percent in the short term to as high as 69 percent with 2-year follow-up. Vacuum constriction devices are more popular in older age group couples, but require substantial enthusiasm and understanding partners. Adverse effects include bruising, obstructed and occasionally painful ejaculation, pain at the site of the ring and penile instability due to pivoting of the base of the penis.
Surgical treatment.
Surgical treatment of “E-D” is usually limited to patients with major penile arterial or venous disease, corporal fibrosis or Peyronie disease, who are either unresponsive to or are not candidates for “E-D” pharmacotherapy. Multicomponent inflatable penile implants are associated with high satisfaction rates. Device failure and prosthetic infection are uncommon. Infection requires removal of the prosthesis and either immediate replacement or delayed staged re-implantation.
Penile arterial revascularisation and venous ligation surgery are associated with relatively poor outcome results in men with penile atherosclerotic disease or corporal veno-occlusive dysfunction. They are rarely required, with the exception of young men with traumatic occlusion or stenosis of the internal pudendal or common penile artery due to an anterior open book type pelvic fracture.
Management of erectile dysfunction after treatment for prostate cancer.
“E-D” is a common consequence of treatment for prostate adenocarcinoma with a radical retropubic prostatectomy, external beam radiotherapy, brachytherapy or androgen deprivation. The aetiology of “E-D” after radical retropubic prostatectomy includes operative injury to the cavernous nerves and subsequent increased hypoxia-induced production of transforming growth factor-beta1 (TGF-beta1) in the corpora cavernosa, leading to increased extracellular matrix deposition, inhibition of smooth muscle growth, apoptosis of corporal smooth muscle, fibrosis and, eventually, structurally based corporeal veno-occlusive dysfunction. Initial failure to respond to PDE5i is almost universal, but treatment with self-administered intracavernous injection therapy has a high response rate and an increased prospect for subsequent response to PDE5i and eventual restoration of spontaneous erections. Recovery of cavernous nerve function is more likely in men aged less than 60 years who have normal pre-operative erectile function and have nerve sparing surgery, but may be protracted resulting in a failure to respond to PDE5i for as long as 24 to 36 months. There is early evidence to support a potential rehabilitative role for daily PDE5i as an adjunct to initial treatment with intracavernous injection therapy in promoting the return of erectile function in men undergoing nerve-sparing radical retropubic prostatectomy.
“E-D” after external beam radiotherapy and or brachytherapy is insidious and progressive and is due to radiation-induced microvascular endarteritis of the penile arteries, possible acceleration of pre-existing atherosclerosis and or proximal corporal fibrosis. The response rate to PDE5i is similar to age-matched “E-D” controls. Androgen blockade with androgen receptor blocking drugs (cyproterone acetate, flutamide, bicalutamide) or luteinising hormone-releasing hormone agonists (goserelin, leuprorelin) is often associated with hypoactive sexual desire, “E-D”, delayed ejaculation, anejaculation and anorgasmia. “E-D” due to androgen blockade can be a challenge to treat, although treatment is often not requested due to hypoactive sexual desire. The response to PDE5i is reduced as the low testosterone levels reduce expression of both the nitric oxide synthase (NOS) gene and the PDE5 gene and downregulate PDE5 isoenzyme. Similarly, the response to self-administered intracavernous injection therapy is also reduced.
Conclusion.
“E-D” is a common complaint and is associated with a reduced quality of life for the patient and their partner. This condition is linked to several risk factors, including obesity, lack of exercise, diabetes mellitus, hypertension, dyslipidaemia, cardiovascular disease and cigarette smoking. Furthermore, “E-D” may be the initial sign of generalised endothelial dysfunction and is a predictor of overall cardiovascular health and silent myocardial ischaemia. Treatment with “E-D” pharmacotherapy alone or in combination with graded psychosexual therapy is effective in improving and or restoring sexual function in most men. Overall, there is a high level of consensus on the management of “E-D” in the selected guidelines with few inconsistencies.
Competing interests and Sixty Nine References.
-
 LIVE
LIVE
BEK TV
22 hours agoTrent Loos in the Morning 7/24/2025
369 watching -
 7:02
7:02
China Uncensored
14 hours agoWell, I Guess Now We Know...
9.63K16 -
 46:10
46:10
Members Club
17 hours agoThe WNBA Has Demands, TSA Loosens Up, and NYC Has a Whale Whisperer - MC04
8.36K1 -
 1:35:15
1:35:15
Man in America
14 hours ago🚨 ALERT: Hospitals in the U.S. Are KILLING Patients… for Their Organs!
81.6K33 -
 8:00
8:00
DropItLikeItsScott
14 hours agoIs This The BEST SIG P365? SIG P365 FUSE
2.42K -
 11:55
11:55
The Shannon Joy Show
13 hours ago🔥Babies Aborted for Cash.🔥
2.49K -
 6:24
6:24
Zach Humphries
14 hours agoBreaking Crypto News on Crypto Regulation!
3.92K3 -
 15:41
15:41
BaldBrad
15 hours agoDeclassified BOMBSHELL: CIA Lied About Trump-Russia! Putin Never Backed Trump | Russiagate Exposed
3.67K5 -
 13:07
13:07
Nate The Lawyer
16 hours ago $0.70 earnedWNBA Loses $500M But Players Want More Money. $40M Lost Last Year.
8.46K6 -
 11:43
11:43
Zoufry
18 hours agoThe McDonald's Ice Cream Machine Conspiracy
7.33K3