Premium Only Content
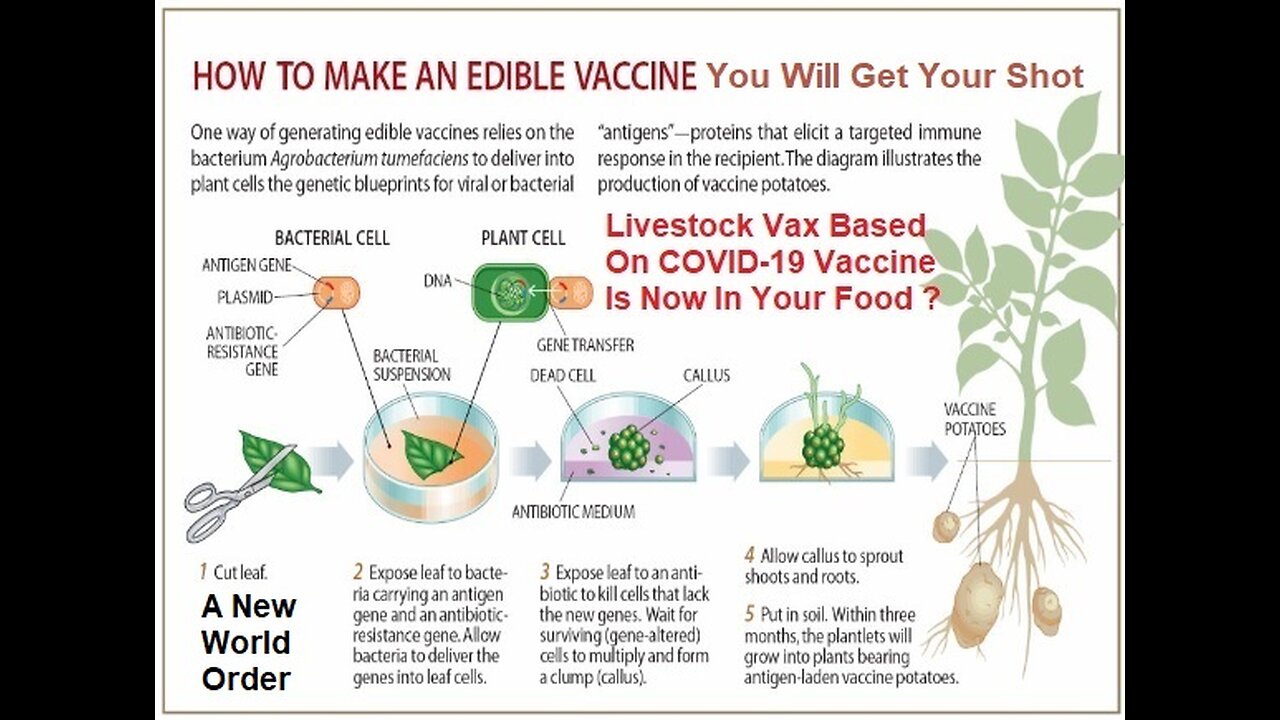
What’s in a Covid-19 Vaccine? - Everyone Will Now Get Edible Vaccine in Your Food
Plant biologist injecting tiny amounts of virus into tomato, potato, lettuce leaves. University of Ottawa plant biologist Allyson MacLean demonstrates the process for injecting edible plants with bacterial solution, which will hopefully cause the leaves to gradually produce a vaccine for COVID-19. Eating your veggies isn't only good for you — it may someday protect you against COVID-19.
That's the hope of a plant biologist at the University of Ottawa who's working to create an edible vaccine for the novel coronavirus. Allyson MacLean's research involves injecting tomato, potato and lettuce plants with a tiny particle of viral DNA swimming in a bacterial solution.
"We take a syringe that does not have a needle point. You press it up against the large leaf … and you basically push … the bacteria into the plant tissues," said MacLean, 41, an assistant professor of plant biology.
The bacteria piggyback that DNA into the plant, which triggers the production of viral proteins. Eating the plant allows these proteins to pass through the digestive system, where they're taken up by special cells in the gut, stimulating a type of immunity.
It's called "mucosal immunity," and it's of particular interest to the scientists currently joined in battle with COVID-19 because the virus that causes the disease, SARS-CoV-2, enters the body via the mucosal surface of the respiratory system.
MacLean has spent a decade researching symbiosis in nature, specifically how microbes and plants co-exist. One of the most common microbes is Agrobacterium tumefaciens, which lives in soil and naturally latches onto plants.
"It finds a wound in the plant and it gets in there. It takes part of its DNA and injects it into a plant cell. It basically makes the plant cells grow tumours … that the bacteria can then use as a food source," MacLean explained.
"People realized a few decades ago that this was going on in nature," she said. "Somebody had the brilliant idea: OK, can we harness this as a way of making genetically modified organisms?"
In her current research to create an edible vaccine for COVID-19, MacLean is using "parts of the virus that other researchers believe will elicit a strong protective antibody response." They're catching a ride into the plant tissue on the back of her old friend Agrobacterium.
At this point in the research, MacLean is using a close relative of tobacco to determine the best way to make a plant express the viral proteins. Next stop, lettuce.
The pandemic hasn't made MacLean's research easy. When COVID-19 struck in March, she struggled to move her hands-on laboratory course online, and began alternating work days with her husband so they could care for their two children, ages one and four.
"It was having to simultaneously balance unprecedented challenges in terms of research, in terms of teaching and in terms of myself as a parent," MacLean said. "It was really hard."
She was especially worried about her "precious transgenic mutant plants" that were left behind in the lab when the U of O campus was shut down due to COVID-19.
"You can't just stop caring for them or you will lose them," said MacLean, who arranged permission to feed and fertilize the plants three times a week.
MacLean had an early fascination with biology and ecology. As a child, she set up a dragon fly hospital in her bedroom, catching flies for her patients' dinner. She harboured a garter snake in her closet one winter. She remembers dabbing a drop of liquid paper on toads in her backyard to see if she could trace their movements.
"I always very much loved living organisms. They just got smaller," she said. There are a few conventional COVID-19 vaccines already at the human trial stage, but "it's premature to stop exploring other avenues," said MacLean — especially if the outcome is a more efficient route to global immunity.
"Plant-based vaccines are better for the developing world. They're cheaper to produce. They don't need … to be refrigerated for long periods of time." Plus, she believes people would rather eat their medicine than get a shot. "People are more willing to ingest a vaccine than they are to get a needle."
MacLean's work will be tested on mice in collaboration with John Bell of the Ottawa Health Research Institute. "This project is pairing up a cancer researcher who uses viruses to tackle cancer and a plant biologist who normally studies the way microorganisms interact with plants," MacLean said. "We're both stretching out of our comfort zones."
Covid-19 vaccine side effect leaves women questioning why birth control pill is not safer Concerns over blood clotting in connection with Covid-19 vaccines have raised questions around why birth control pills.
In April, as the Food and Drug Administration paused use of Johnson & Johnson’s Covid-19 vaccine to evaluate the risk of blood clots in women younger than 50, many scientists noted that clots associated with birth control pills were much more common.
The comparison was intended to reassure women of the vaccine’s safety. Instead, it has stoked anger in some quarters — not about the pause, but about the fact that most contraceptives available to women are hundreds of times riskier, and yet safer alternatives are not in sight.
The clots linked to the vaccine were a dangerous type in the brain, while birth control pills increase the chances of a blood clot in the leg or lung — a point quickly noted by many experts. But the distinction made little difference to some women.
“Where was everyone’s concern for blood clots when we started putting 14-year-old girls on the pill,” one woman wrote on Twitter.
Another said, “If birth control was made for men, it’d taste like bacon and be free.”
Some women heard, on social media and elsewhere, that they should not complain because they had chosen to take birth control knowing the risks involved.
“That just made me double down,” said Mia Brett, an expert in legal history focused on race and sexuality at Stony Brook University in New York. “This is such a common response to women’s health care — that we point out something and it’s dismissed.”
‘They should be angry’
The torrent of fury online was familiar to experts in women’s health.
“They should be angry — women’s health just does not get equal attention,” said Dr Eve Feinberg, a reproductive endocrinologist and infertility specialist at Northwestern University. “There’s a huge sex bias in all of medicine.”
Feinberg and many of the women online acknowledge that contraceptives have given women control over their fertility, and the benefits far exceed the harms.
Rebecca Fishbein, a 31-year-old culture writer, started tweeting about the inadequacy of birth control pills almost immediately after the announcement of the pause.
Still, “birth control is an incredible invention; thank God we have it,” she said in April in an interview. “I’ll fight anyone who tried to take it away.”
‘Overall, it’s incredibly safe’
Contraceptives have also improved over the years, with intrauterine devices and oral options that offer an ultralow dose of oestrogen.
“Overall, it’s incredibly safe,” Feinberg said. “Everything that we do has risks.”
But Feinberg said it was crucial for health care providers to discuss the risks with their patients and coach them on worrisome symptoms — a conversation many women said they had never had.
Kelly Tyrrell, a communications professional in Madison, Wisconsin, was 37 when doctors discovered potentially fatal blood clots in her lungs.
Tyrrell is an endurance athlete — wiry, strong and not prone to anxiety. In early 2019, she began waking up with a pain in her left calf. After one particularly bad morning, an urgent-care visit revealed that she had high blood levels of “D dimer,” a protein fragment that indicates the presence of clots.
She had been taking birth control pills for 25 years, but none of the doctors made a connection. Instead, they said that given her age, fitness and the lack of other risk factors, her symptoms were unlikely to be from a blood clot. They sent her home with instructions to do stretches for her calf muscle.
When she felt a tightness in her chest while running in Hawaii after her grandmother’s funeral, doctors said the cause was probably stress and anxiety.
‘I instantly burst into tears’
In July 2019, she finished a 100K race in Colorado and assumed that her aching lungs and purple lips were the result of running for 19 hours at a high altitude.
But she knew something was seriously wrong on the morning of 24 October, 2019, when she became short of breath after walking up a short flight of stairs.
This time, after ruling out heart problems, doctors scanned her lungs and discovered multiple clots. One had cut off blood flow to a portion of her right lung.
“I instantly burst into tears,” Tyrrell recalled.
The doctors put her on a course of blood thinners — and told her never to touch oestrogen again. Tyrrell switched to a copper IUD. Over time, she added, the incident had escalated into a sharp rage that was renewed by the Johnson & Johnson news.
“Part of my anger was that a medication that I took to control my fertility ended up threatening my mortality,” she said. “I’m angry that I hadn’t been counselled better about that risk, or even what to look for.”
Emily Farris, 36, was prescribed oral contraceptives at age 8 to help with migraines. In all of the conversations she has had with her many doctors over the years, “never once was blood clots brought up,” she said in an interview.
On Twitter, some critics pointed out that the inserts with birth control packs clearly describe the blood clot risk.
“My response is a bit incredulous to that,” said Farris, a political scientist at Texas Christian University in Fort Worth.
The inserts for most medications have a long list of possible side effects, placing “a high burden for folks to try to sort through medical research, to sort through what probability and statistics mean,” she said.
Even with a doctorate-level education, “I can’t assess those risks,” Farris added. “I think most Americans need someone to translate what the legalese kind of pamphlet is into real terms.”
For Tyrrell, that elucidation came much too late. Her lungs have not felt the same since her diagnosis, but she cannot be sure whether that is because of lingering damage from a previous blood clot, new clots that she should be worried about or simply her age, she said, adding: “It’s never not on my mind anymore.”
Following the death of a 32 year woman, who suffered from blood clotting a couple weeks after receiving a Covid-19 vaccine, an obstetrician-gynecologist in Thailand has advised women think about whether to stop taking birth control pills before receiving the Covid-19 vaccines due to a possible increased risk of blood clots.
The doctor spoke during a live streaming session following the death of 32 year old Naririn Angthong. The woman from Thailand’s Deep South province Yala died from blood clotting in her lungs 2 weeks after receiving the Covid-19 vaccine. She was injected with the vaccine on May 14 and died on May 27 at Hat Yai Hospital. The death is still under investigation.
While there’s no evidence that the vaccine will increase the risk of blood clots for women who are taking the daily contraceptive pill, the hormones in the medication increase the risk, according to Siraya Kitiyodom, an OB-GYN at Maharat Nakhon Ratchasima Hospital. She says women who are concerned with potential side effects of the vaccine might want to consider other birth control methods
Another health official in Thailand also advised women to stop taking the pill before receiving a Covid-19 vaccine. The head of the Centre for Emerging Disease Health Sciences at the Faculty of Medicine at Chulalongkorn University, Thiravat Hemachudha, wrote on his Facebook page saying women should should stop taking hormone contraceptive pills at least 14 days before getting vaccinated against the coronavirus. He also said people should stop taking migraine medicine before getting the vaccine.
Researchers aim to develop edible plant-based mRNA vaccines The future of vaccines may look more like eating a salad than getting a shot in the arm. UC Riverside scientists are studying whether they can turn edible plants like lettuce into mRNA vaccine factories.
Messenger RNA or mRNA technology, used in COVID-19 vaccines, works by teaching our cells to recognize and protect us against infectious diseases.
One of the challenges with this new technology is that it must be kept cold to maintain stability during transport and storage. If this new project is successful, plant-based mRNA vaccines -; which can be eaten -; could overcome this challenge with the ability to be stored at room temperature.
The project's goals, made possible by a $500,000 grant from the National Science Foundation, are threefold: showing that DNA containing the mRNA vaccines can be successfully delivered into the part of plant cells where it will replicate, demonstrating the plants can produce enough mRNA to rival a traditional shot, and finally, determining the right dosage.
"Ideally, a single plant would produce enough mRNA to vaccinate a single person," said Juan Pablo Giraldo, an associate professor in UCR's Department of Botany and Plant Sciences who is leading the research, done in collaboration with scientists from UC San Diego and Carnegie Mellon University.
Key to making this work are chloroplasts -; small organs in plant cells that convert sunlight into energy the plant can use. "They're tiny, solar-powered factories that produce sugar and other molecules which allow the plant to grow," Giraldo said. "They're also an untapped source for making desirable molecules."
In the past, Giraldo has shown that it is possible for chloroplasts to express genes that aren't naturally part of the plant. He and his colleagues did this by sending foreign genetic material into plant cells inside a protective casing. Determining the optimal properties of these casings for delivery into plant cells is a specialty of Giraldo's laboratory.
For this project Giraldo teamed up with Nicole Steinmetz, a UC San Diego professor of nanoengineering, to utilize nanotechnologies engineered by her team that will deliver genetic material to the chloroplasts.
"Our idea is to repurpose naturally occurring nanoparticles, namely plant viruses, for gene delivery to the plants," Steinmetz said. "Some engineering goes into this to make the nanoparticles go to the chloroplasts and also to render them non-infectious toward the plants."
For Giraldo, the chance to develop this idea with mRNA is the culmination of a dream. "One of the reasons I started working in nanotechnology was so I could apply it to plants and create new technology solutions. Not just for food, but for high-value products as well, like pharmaceuticals," Giraldo said.
He is also co-leading a related project using nanomaterials to deliver nitrogen, a fertilizer, directly to chloroplasts, where plants need it most.
Nitrogen is limited in the environment, but plants need it to grow. Most farmers apply nitrogen to the soil. As a result, roughly half of it ends up in groundwater, contaminating waterways, causing algae blooms, and interacting with other organisms. It also produces nitrous oxide, another pollutant.
This alternative approach would get nitrogen into the chloroplasts through the leaves and control its release, a much more efficient mode of application that could help farmers and improve the environment.
The National Science Foundation has granted Giraldo and his colleagues $1.6 million to develop this targeted nitrogen delivery technology. "I'm very excited about all of this research," Giraldo said. "I think it could have a huge impact on peoples' lives."
Marijuana and COVID-19: What a Doctor Wants You to Know With the rapid spread of the new coronavirus throughout the globe, people are looking for ways to protect their health and lessen the risk of COVID-19 complications. Because having damaged lungs is one of the main risk factors for complications, smoking of any kind is being discouraged by health experts.
As it's become legal in some parts of the U.S., many people use cannabis products for both medical and recreational purposes, and some who smoke, inhale, or vape marijuana are wondering if it’s safer to switch to alternatives, like “edibles” to protect their lungs and immune systems.
Just like the developing science around COVID-19, the facts around cannabis are also murky. To help me navigate the data, I turned to several scientists behind the 2017 National Academy of Sciences (NAS) report on the health effects of cannabis and related products. According to Daniele Piomelli, PhD, professor of anatomy and neurobiology, and Chair in Neuroscience at the University of California, Irvine School of Medicine, “we don’t have a lot to go on” when it comes to marijuana and the risk for viral infections like COVID-19, but there are definitely some steps we can take when it comes to reducing harms from marijuana use.
Are edibles (and other non-inhaled forms) safer than smoking marijuana?
There is a lot of evidence that points to an association between long-term cannabis smoking and lung damage causing chronic cough and phlegm production. There’s also evidence that when you stop, these lung symptoms can improve. “Are edibles safer than smoked cannabis? Yes, they are safer to the lung – that is a slam dunk,” says Piomelli. He stresses, however, that they are not risk free. He points out that it is almost impossible to know for sure how much THC (the active ingredient that gives the “high”) is in edible forms like gummies and chocolates because manufacturers are not bound by rules to abide by what is listed on the label. (While this is the case in most states, several states that have legalized cannabis use require that manufacturers lab test products to ensure the dosage information on the label is accurate for all legally sold products.)
When someone smokes, they have a much better sense of when to stop based on how they are feeling. This is not the case for edibles, says Piomelli. “One or two hours later, all of a sudden, it can hit like a sledgehammer – you can have a ‘bad trip’ (and) once you have it there is no undoing it. You have to wait it out until it is metabolized and out of your system.” Side effects from overdose, like paranoia, panic, and nausea are mostly a risk for people who are switching to new products, where people don’t know how their bodies will react. Another important point is that edibles usually are high in sugar, which is not ideal for maintaining a healthy lifestyle.
Does cannabis have beneficial effects that help with anxiety?
There is growing concern about the mental health impacts of the coronavirus pandemic. Add social isolation from strict lockdowns to economic stressors, and there is growing evidence that people are looking for ways to curb their anxiety.
A recent study showed that prescriptions for anti-anxiety medications, anti-depressants, and anti-insomnia medicines increased after the WHO declared a global pandemic. There’s also evidence that alcohol sales and alcohol consumption have increased during this time.
Piomelli says “It’s understandable that people may be using more cannabis at home these days. Once the numbers are found out, we will have more data on this.” He suggests that cannabis products that people are comfortable and familiar with may be reasonable in moderation, and are likely safer than alcohol and other psychoactive substances. According to the NAS report, people should be aware, however that regular, long-term use may increase the risk for developing social anxiety disorder and heavy users are more likely to report thoughts of suicide.
It’s also important to realize that if you are using cannabis to “self-medicate” for anxiety, you should reach out to a professional for help.
How does cannabis affect the immune system?
Given the COVID-19 pandemic, there’s a lot of interest around maintaining a healthy immune system. The NAS report delved into the evidence around the effects of cannabis on the immune system and the susceptibility to viral infections.
There is an intriguing finding noting a small body of evidence that shows that cannabis may decrease the production of several inflammatory cytokines (immune system proteins). This is an important area of study right now, because scientists have found that in many of the most severe cases of COVID-19, there seems to be an over-production of these cytokines, also known as “cytokine storm,” which prompts the body to attack its own cells and tissues instead of fighting the virus.
It’s really important to know, however, that the immune system is made up of a variety of cells and chemical signalers that interact through a complex interplay, so it’s hard to say where cannabis may help tamp down the immune system and where it may hurt by increasing the risk of infection.
Piomelli points out that a few more scientific papers have been released since the 2017 NAS report looking at cannabis and viral infections. One particular study looked at the evidence not only around THC containing cannabis but also cannabidiol (CBD). CBD is also found in the cannabis plant, but unlike THC, does not have the properties that cause the “high.” The findings from this study are encouraging and will hopefully prompt further study because there may be a chance that CBD can help control inflammation and help manage certain viruses – but the evidence is still scant.
“The point is we don’t enough data. I wish we did,” says Piomelli.
Major takeaways:
Inhaling, smoking, or vaping cannabis products in the face of COVID-19 is not recommended.
If cannabis use is legal where you live and you want to switch to edibles or other forms of cannabis, make sure it’s a known entity that you have experience with, and use only in moderation. (Remember that these products can be high in sugar content.)
With edibles, there is a higher risk of a “bad trip,” especially for those who have not used them in the past.
There is not enough evidence to know the effects of cannabis on the immune system or on the susceptibility to viral infections.
Consider other ways of managing anxiety. Creating a routine that includes exercise, proper nutrition, meditation, and regular social interactions can help manage stress in a healthy way.
If you are using cannabis to treat anxiety, reach out for help from a mental health professional
Editor's note: This post has been updated to acknowledge that edibles may be regulated in some states.
COVID-19 vaccines: Get the facts
Looking to get the facts about COVID-19 vaccines? Here's what you need to know about the different vaccines and the benefits of getting vaccinated.
As the coronavirus disease 2019 (COVID-19) pandemic continues, you might have questions about COVID-19 vaccines. Find out about the different types of COVID-19 vaccines, how they work, the possible side effects, and the benefits for you and your family.
https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-vaccine/art-20484859
COVID-19 Vaccines Will Kill You ? Animation What Happens If You Get Coronavirus Effect - https://rumble.com/v2dt6zk-covid-19-vaccines-will-kill-you-animation-what-happens-if-you-get-coronavir.html - These studies help prove that receiving the COVID-19 vaccine before or during pregnancy is not associated with higher rates of miscarriage. Nevertheless, more research is needed to strengthen the evidence-base and combat persistent misinformation. Continued investment and investigation is critical to fighting vaccine hesitancy and preventing the further spread of COVID-19, especially among vulnerable populations.
Click on the links below for the full story and or Type it into a Web Base Search !
https://www.exposingtheirlies.com/post/some-covid-19-horror-stories-you-may-have-missed
WHO’s DoV vision led to a collaboration in which Bill Gates’ GAVI serves on the leadership council. The Global Vaccine Action Plan (“GVAP”) – endorsed by the 194 Member States of the World Health Assembly in May 2012 – came out of the collaboration. The “leadership” that produced the GVAP are the Bill & Melinda Gates Foundation, GAVI Alliance, UNICEF, United States National Institute of Allergies and Infectious Diseases and the World Health Organization (“WHO”).
Livestock Vax Based On COVID-19 Vaccine Technology Raises Concerns A livestock vaccine using the same technology as the COVID-19 vaccine hasn’t been approved for use, but some legislators are moving to implement labeling rules on foods coming from animals that receive the vaccine. A molecular biologist said the vaccine can’t get into the foods being labeled.
Pharmaceutical companies are developing vaccines for livestock that work using the same technology as the COVID-19 vaccine.
Vaccines are a sensitive topic for many, and though none of these livestock vaccines have been approved for use in the U.S., some lawmakers are introducing legislation to label meats that come from animals that have received these vaccines.
A molecular biologist said these laws are unnecessary and misleading, because the vaccines can't get into the food supply.
How They Work
The vaccines work by introducing a piece of messenger RNA (mRNA) that corresponds to a viral protein. The mRNA doesn't enter the nucleus of the cell and cannot alter DNA. Using the mRNA, cells produce the viral protein, and the immune system, as part of its normal response, produces antibodies that fight off future infections.
Currently, the COVID-19 vaccine is the only mRNA approved for use in the U.S. on humans.
Lawmakers in Arizona, Idaho, and Missouri have introduced legislation related to the use of mRNA vaccines in food. The Arizona bill only restricts labeling such food as organic. The Idaho bill amends state law to prohibit the sale of such foods unless conspicuously labeled that the presence of the vaccine is in the food.
The Missouri bill requires a conspicuous "Gene Therapy Product" label.
Dr. Kevin Folta told Cowboy State Daily the proposed "gene therapy" label is inaccurate.
It "means they have no idea what they are trying to regulate," Folta said, because "there is no integration into the DNA. Its a transient set of instructions, like a USB drive. Not a hard drive."
Folta is a professor of the horticultural sciences in the horticultural sciences department of the University of Florida. He has a Ph.D. in molecular biology from the University of Illinois in Chicago. He's been an outspoken advocate against claims that genetically modified organisms are unsafe or that the use of pesticides and herbicides cause negative health impacts.
mRNA-Free Cows
To illustrate the lack of accurate information on these livestock vaccines, Folta recently tweeted a photo of a cow stating it was happily "mRNA free."
Messenger RNA occurs naturally as part of the function of cells in the body.
"mRNA is everywhere, and you cant live without mRNA," Folta said.
Folta explained that the mRNA vaccines could save the cattle industry billions every year. There are a number of viral diseases, including hoof and mouth disease, pseudorabies and avian influenza.
The vaccines, Folta explained, are used to vaccinate the animals against these and other highly contagious diseases.
Some of these diseases are zoonotic, meaning humans can get them from animals, such as rabies, avian influenza, and lyme disease. The vaccines can also prevent the diseases from jumping from livestock to wildlife, which can be very susceptible to epidemics.
Unfortunate Situation
His efforts to communicate accurate science on agriculture issues have made him the target of organic food advocates.
They accuse him of receiving funding from biotech companies.
The Organic Consumers Association funded a campaign to file multiple Freedom of Information Act requests with the University of Florida to delve into Folta's emails, hoping to prove that he was paid by biotech companies to communicate his science-based perspectives.
Nothing was ever found indicating he had committed any scientific misconduct.
The campaign was such a drain on resources in the department that he was asked to cease his speaking engagements and just teach classes. He said he's been able to come to an understanding with the university.
"It really is an unfortunate situation because we were making some really good progress," Folta said.
Folta said that the vaccines can't get into the food people eat.
"mRNA is an extremely unstable molecule. That's why it works. It's very temporary. So when an animal is slaughtered or when a plant dies, mRNA is the first thing to go," Folta said.
He said it can't be stable at room temperature or when it's not being actively produced.
Besides its instability, it's injected into a localized area on the animal.
Because the vaccines can protect livestock herds from illness, the cattle industry is interested in the mRNA vaccines, Folta said.
When it comes to communicating their safety, Folta said, the benefit to ranchers isn't always convincing because it runs up against a lot of anti-agricultural bias. He tries to stress the benefits to wildlife and humans.
"There's way too much of that [anti-agriculture bias] out there. But the same people who don't like farmers sure do like conservation. So we can protect wild populations and humans," Folta said.
Transparency Labeling
Missouri State Rep. Holly Jones, who sponsored the Missouri bill, told Cowboy State Daily that the legislation doesn't ban the use of the vaccines.
"The public deserves to understand what is in their food supply," Jones said.
She said that mRNA technology is being used without the right amount of studies on safety and efficacy, and she doesn't think the "gene therapy" label would be problematic. Jones said that we already have labels we put on products, such as "grass-fed beef" and "non-GMO."
"There needs to be something specific to gene therapy labeling, especially when it comes to our food supply," Jones said. "We have to be specific enough that people understand what they're putting in their body. I believe consumers deserve to have that information."
Jones said that her bill would support farmers who would become vulnerable to lawsuits without those labels.
"This is actually pro-business," Jones said.
Catastrophic
Brett Moline, director of public and governmental affairs for the Wyoming Farm Bureau Federation, told Cowboy State Daily that the vaccines in use today are vital to the livestock industries.
When the cows are branded, they get a set of shots to protect them from diseases.
"What's keeping the diseases from being on the front page is we don't have outbreaks of diseases, like black leg. You just don't hear about them anymore," Moline said.
The health of the animals is important to producers and their bottom line, Moline said, and so keeping disease under control is part of the business. With profits in the industry on the margin, every animals health counts. "Happy cows make ranchers happy. To take away that tool could be just catastrophic," Moline said.
COVID-19 AND BEEF FREQUENTLY ASKED QUESTIONS
Q: Are animals responsible for COVID-19 in people?
The predominant route of transmission of COVID-19 appears to be from human to human.1
According to the CDC, there is no evidence that animals, including pets, play a significant role in spreading the virus that causes COVID-19.
In isolated cases, it appears the virus can spread from people to animals, though further research is needed to understand how animals could be affected by COVID-19. Based on limited information available, the risk of the virus spreading between animals and people is considered low.9
Current evidence suggests that the COVID-19 virus has an animal source. Ongoing investigations are important for identifying the animal source. To date, there is not enough scientific evidence to identify that source or to explain the route of transmission from an animal source to humans.1
Q: Can the bovine coronavirus vaccine be used to treat people?
Bovine coronavirus is NOT the same as COVID-19.
There is no evidence to suggest that the bovine coronavirus vaccine has any effect on humans or the COVID-19 strain. Vaccines are developed and tested for specific strains of viruses and species and should only be used according to label instructions. 2, 3
The bovine coronavirus, as the name suggests, is specific to cattle and other domestic animals (i.e., horses, water buffalo, deer, elk, etc.). There is no cross protection between bovine coronavirus and COVID-19. 2, 3
There are currently no antiviral drugs recommended or licensed by FDA to treat COVID-19, and there is no immunization available.4
Q: Will beef from cattle vaccinated for bovine coronavirus help build immunity against COVID-19?
There is no evidence to suggest that this is the case.
Even if a vaccine for bovine coronavirus is used in cattle, there is a 21-day or 60-day meat withdrawal period, depending on the vaccine, required prior to processing. This ensures the end product is safe for consumption and no medication would be present in the beef.5
Q: What impact is COVID-19 having on the beef supply?
Cattle farmers and ranchers continue to produce high-quality beef.
As COVID-19 continues to spread and impact economic activity, there is a great deal of uncertainty in terms of what it means for the beef industry, including on supply and demand.
At this time, it’s impossible to measure the full effects of the virus or determine how it may continue to unfold.
Q: How does bovine coronavirus affect cattle?2, 3
Bovine coronavirus is a cattle virus that farmers and ranchers have vaccinated their cattle against and managed for years. It can manifest as either a respiratory infection or gastrointestinal disease in cattle of all ages.
Gastrointestinal signs include profuse diarrhea, dehydration, depression, reduced weight gain and anorexia.
Bovine coronavirus has been associated with upper and lower respiratory tract disease and is a component of Bovine Respiratory Disease Complex. Signs may include respiratory distress, fever, nasal discharge, and coughing.
Like other viral infections, other factors can influence an animal’s risk of infection and its ability to overcome the infection. These include host factors such as immunologic status or coinfections with a secondary bacterial infection and environmental factors such as extreme cold or hot temperatures.
Q: How do farmers and ranchers care for the cattle if they are sick with bovine coronavirus?5
Farmers and ranchers use a variety of tools, including vaccines, good nutrition programs, low-stress handling, and proper housing to keep animals healthy.
If necessary, antibiotics may be a tool that farmers and ranchers use to treat an animal.
Beef farmers and ranchers work with veterinarians and animal health experts to ensure antibiotics are used responsibly.
The beef community has significantly invested in educational programs, like Beef Quality Assurance and research to maintain high standards of animal care and health, including continuously improving the stewardship of antibiotics used in cattle.
Q: What is Beef Quality Assurance (BQA)?5
Developed in 1991, Beef Quality Assurance (BQA) is a voluntary certification program that provides the U.S. beef industry with a consistent set of animal welfare standards and best practices.
The BQA program exemplifies what beef farmers and ranchers have always cared about – a commitment to caring for their animals and providing families with the safest and highest-quality beef possible.
Consumers can feel good knowing there’s a national program in place that sets consistent animal welfare and care standards across the beef industry. The result is wholesome safe, high-quality meat.
More than 85 percent of the beef supply in the U.S. comes from farms and ranches that adhere to BQA standards and guidelines, and this number continues to increase monthly.
The BQA program is nationally coordinated by the National Cattlemen’s Beef Association (NCBA), a contractor to the Beef Checkoff.
Q: Can I become sick with COVID-19 from food?
USDA is not aware of any reports at this time of human illnesses that suggest COVID-19 can be transmitted by food or food packaging. However, it is always important to follow good hygiene practices (i.e., wash hands and surfaces often, separate raw meat from other foods, cook to the right temperature, and refrigerate foods promptly) when handling or preparing foods.6
According to the World Organization for Animal Health (OIE), meat from healthy livestock that is prepared and served in accordance with good hygiene and food safety principles remains safe to eat.1
Q: Are meat products compromised by COVID-19?
USDA is not aware of any reports at this time of human illnesses that suggest COVID-19 can be transmitted by food or food packaging. However, it is always important to follow good hygiene practices (i.e., wash hands and surfaces often, separate raw meat from other foods, cook to the right temperature, and refrigerate foods promptly) when handling or preparing foods.6
According to the World Organization for Animal Health (OIE), meat from healthy livestock that is prepared and served in accordance with good hygiene and food safety principles remains safe to eat.1
Q: Are food products produced in the United States a risk for the spread of COVID-19?
There is no evidence to suggest that food produced in the United States can transmit COVID-19.6
According to the World Organization for Animal Health (OIE), meat from healthy livestock that is prepared and served in accordance with good hygiene and food safety principles remains safe to eat.1
Q: Can I get sick with COVID-19 from touching food, the food packaging, or food contact surfaces, if the coronavirus was present on it?
Currently there is no evidence of food or food packaging being associated with transmission of COVID-19. Like other viruses, it is possible that the virus that causes COVID-19 can survive on surfaces or objects. For that reason, it is critical to follow the 4 key steps of food safety — clean, separate, cook, and chill.6
Q: If an inspector or worker in a meat processing plant became infected with coronavirus, would the meat produced at that facility be safe to eat?
Public health and food safety experts do not have any evidence to suggest that COVID-19 can be transmitted by food or food packaging. FSIS in-plant personnel who are ill with COVID-19 or any other illness will be excluded from work activities that could create unsanitary conditions (coughing or sneezing on product). COVID-19 is thought to spread mainly from person to person through respiratory droplets that can land in the mouths or noses of people who are nearby.1, 6
Q: Can companion animals spread COVID-19?
Currently, there is no evidence to suggest that animals infected by humans are playing a role in the spread of COVID-19. Human outbreaks are driven by person to person transmission.1
Studies are underway to better understand the susceptibility of different animal species to the COVID-19 virus and to assess infection dynamics in susceptible animal species.
Preliminary findings from laboratory studies suggest that, of the animal species investigated so far, cats are the most susceptible species for COVID-19, and, in a laboratory setting, cats were able to transmit infection to other cats. Ferrets also appear to be susceptible to infection but less so to disease. In the laboratory setting ferrets were also able to transmit infection to other ferrets. Dogs appear to be susceptible to infection but appear to be less affected than ferrets or cats.i1
While there are currently no reports of cattle testing positive for COVID-19, now that COVID-19 virus infections are widely distributed in the human population there is a possibility for some animals to become infected through close contact with infected humans or a fomite that carries the virus for a short time.i1
Further studies are needed to understand if and how different animals could be affected by COVID-19. State animal and public health officials are working closely with USDA and CDC to monitor this situation and will conduct additional testing if it is warranted.8
Q: Could a farmer or rancher with COVID-19 infect cattle with the virus?
While there are currently no reports of cattle testing positive for COVID-19, now that COVID-19 virus infections are widely distributed in the human population there is a possibility for some animals to become infected through close contact with infected humans.1
Further studies are needed to understand if and how different animals could be affected by COVID-19. State animal and public health officials are working closely with USDA and CDC to monitor this situation and will conduct additional testing if it is warranted.
Anyone sick with COVID-19 should restrict contact with animals out of an abundance of caution during their illness, just as they would with other people. Although there have not been reports of animals beyond a tiger at the Bronx zoo becoming sick with COVID-19 in the United States, it is still recommended that people sick with COVID-19 limit contact with animals until more information is known about the virus. If a sick person must care for a pet or be around animals, they should wash their hands before and after the interaction.
Q: If cattle were to become infected with COVID-19, would beef from those animals be safe for human consumption?
There are currently no reports of cattle testing positive for COVID-19.
The USDA is not aware of any reports at this time of human illnesses that suggest COVID-19 can be transmitted by food or food packaging. However, it is always important to follow good hygiene practices (i.e., wash hands and surfaces often, separate raw meat from other foods, cook to the right temperature, and refrigerate foods promptly) when handling or preparing foods.6
According to the World Organization for Animal Health, meat from healthy livestock that is prepared and served in accordance with good hygiene and food safety principles remains safe to eat.1
Q: Did animal agriculture contribute to the emergence of COVID-19?
Current evidence suggests that the COVID-19 virus has an animal source. Ongoing investigations are important for identifying the animal source. To date, there is not enough scientific evidence to identify that source or to explain the route of transmission from an animal source to humans.1
There is no evidence that cattle contributed in any way to the introduction of COVID-19 to humans.
Coronaviruses that infect animals can sometimes be spread to people, but this is rare.9
Q: Could animal agriculture lead to future zoonotic-based pandemics?
The best way to prevent future zoonotic-based pandemics is universal adoption of CDC’s One Health approach to disease control. One Health is a collaborative approach that works at local, national and global levels to recognize the interconnections between people, animals, plants, and their shared environments.
The World Organization for Animal Health envisions One Health as a collaborative global approach for understanding risks for human and animal health. It builds on intergovernmental standards for One Health by publishing worldwide information on animal health collected through country reporting as well as a network of international disease experts and programs for strengthening the capacity of national veterinary service programs.
Since 2012, NCBA has been involved with the activities of the One Health Academy in Washington, DC, which meets monthly to allow for information exchange and policy discussions related to One Health topics.
Q: Could a disease like COVID-19 originate in the U.S. in the future? How does the U.S. prevent zoonotic diseases?
While One Health is an approach recommended globally by the United Nations and World Bank, in the U.S. both the USDA and CDC operate offices of One Health that provide interagency communication, education, and mitigation measures surrounding emerging and zoonotic diseases that could threaten the U.S. Both of these government agencies also collaborate on several well-established and important zoonotic disease surveillance programs.
Throughout its history, the USDA has played a central role in protecting the health of U.S. animal agriculture through essential services involving risk assessment, port of entry inspection for imported animals and agricultural products, regulation of biological agents, development of animal vaccines, performing state-of-the-art animal diagnostic testing, and delivery of comprehensive disease surveillance, control, and eradication.
The U.S. has a proven history of controlling zoonotic diseases as evidenced by measures put into place to address bovine tuberculosis and brucellosis in the 1900s. Today, the U.S. is considered essentially free of these diseases. 10, 11
In the U.S., in addition to work done by USDA and CDC to address emerging and zoonotic diseases that could threaten human and animal health, the beef industry’s Beef Quality Assurance (BQA) program establishes that every member of the beef production system adheres to high standards of care in every aspect of production to deliver healthy animals and high-quality beef.
All types of cattle operations work with a veterinarian to create a customized care plan for their animals. These high-quality care plans contribute to healthier animals with less risk of becoming ill by addressing nutrition, animal husbandry, vaccination plans to prevent disease and low-stress animal handling techniques.
Q: Do feedyards or other cattle operations where a large number of cattle are in close contact increase the likelihood of a zoonotic disease or outbreak originating and/or spreading?
The U.S. is very good at controlling zoonotic diseases as evidenced by measures put into place to address bovine tuberculosis and brucellosis in the 1900s. Today, the U.S. is considered essentially free of these diseases.10, 11
Programs like Beef Quality Assurance (BQA) provide a total quality assurance program that establishes that every member of the beef production system adheres to high standards of care in every aspect of production to deliver healthy animals and high quality beef.
All types of cattle operations work with a veterinarian to create a customized care plan for their animals. These high-quality care plans contribute to healthier animals with less risk of becoming ill by addressing nutrition, animal husbandry, vaccination plans to prevent disease and low-stress animal handling techniques.
Q: Would reducing meat consumption lower the risk of future zoonotic diseases and pandemics?
No. Whether for food or other purposes, interactions between animals and humans occur globally. The best way to prevent future zoonotic-based pandemics is universal adoption of a One Health approach to disease control. One Health is a collaborative approach that works at local, national and global levels to recognize the interconnections between people, animals, plants, and their shared environments.
-
 1:09:00
1:09:00
What If Everything You Were Taught Was A Lie?
24 days agoThe Nazi True 8 Secret SS Base's Vs. American Battle For Antarctica Full Top Secret Story Explained
2.88K4 -
 1:11:30
1:11:30
Sean Unpaved
2 hours agoCowboys Chronicle: Jerry Jones, Micah Parsons, & the NFC East Battle
20.6K -
 1:53:23
1:53:23
Tucker Carlson
2 hours agoMargaret Roberts Exposes the True Story of the Oklahoma City Bombing and the Ongoing Cover-Up
20.3K50 -
 6:09:03
6:09:03
JuicyJohns
6 hours ago $2.20 earned🟢#1 REBIRTH PLAYER 10.2+ KD🟢$500 GIVEAWAY SATURDAY!
60.7K2 -
 LIVE
LIVE
Viss
3 hours ago🔴LIVE - The Energy, The Tactics, and The Knowledge You Need To Win! - PUBG
150 watching -
 1:00:44
1:00:44
RalliedLIVE
1 hour agoWARZONE CHALLENGES WITH DRDISRESPECT & BOB
1.88K1 -
 1:01:03
1:01:03
Timcast
3 hours agoDemocrats SABOTAGE Texas REDISTRICTING, May Be CHARGED
160K129 -
 1:59:07
1:59:07
The Charlie Kirk Show
3 hours agoTexas Dems In Flight + Recess Appointments Or Not? | Sen. Mullin, Halperin, Sen. Scott | 8.4.2025
65.7K19 -
 25:36
25:36
The Quiet Part
5 hours agoThis Is How It Ends—Carney’s EU Obsession Will COLLAPSE Canada
4.25K3 -
 13:37
13:37
Adam Does Movies
17 hours ago $0.30 earnedWar Of The Worlds Is The Worst Movie Of 2025 - Review
3.29K3